Anatomy and Physiology
- Anatomy
- Arterial Supply
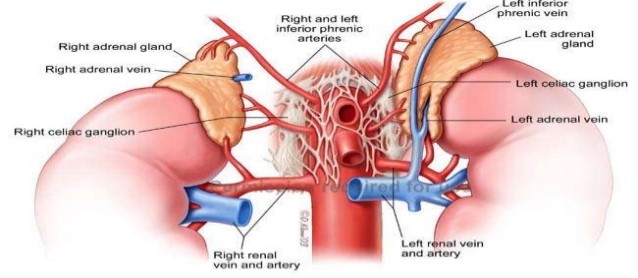
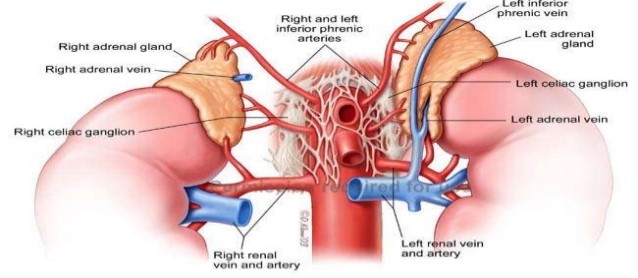
- arises from 3 vessels:
- superior adrenal arteries arise from the inferior phrenic arteries
- middle adrenal arteries arise from the aorta
- inferior adrenal artery arises from the renal artery
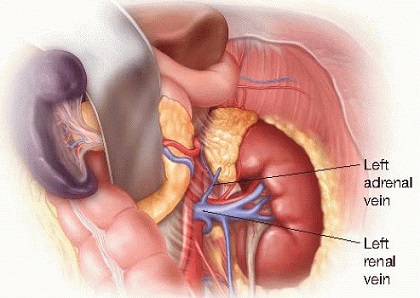
- Venous Drainage
- usually consists of a single vein
- the right adrenal vein is wide and short, and drains into the posterolateral IVC
- the left adrenal vein is long, and drains into the left renal vein
- on the right, venous anomalies occur 20% of the time, with drainage into the right hepatic
vein being the most consequential
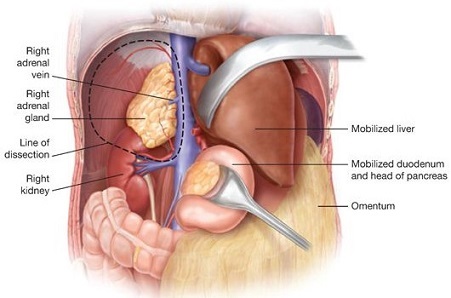
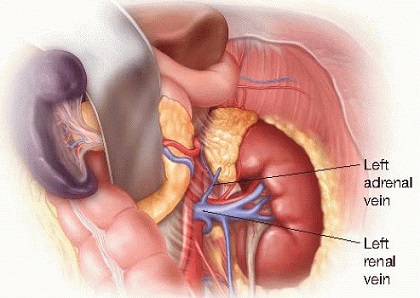
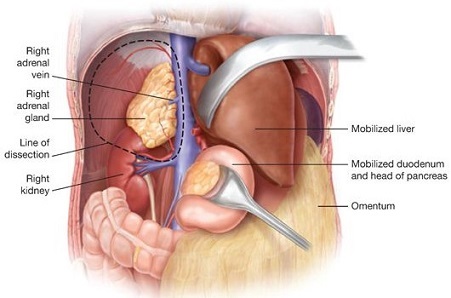
- Anatomic Relationships
- to expose the right adrenal, the hepatic flexure, duodenum (Kocher maneuver), and right
lobe of the liver must be mobilized
- to expose the left adrenal, the splenic flexure must be mobilized inferiorly, and the spleen
and pancreas must be mobilized superiorly and medially
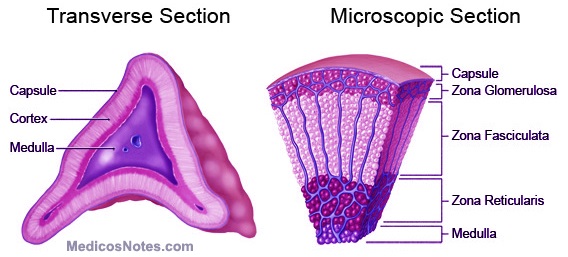
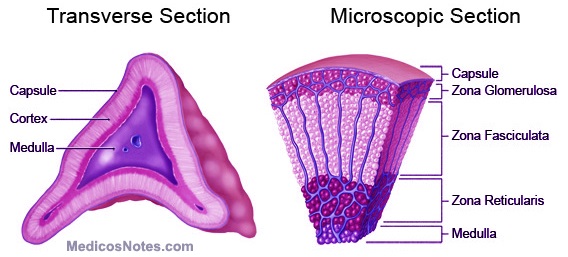
- Histology
- consists of an outer cortex and inner medulla
- Cortex
- comprises 80% of the mass of the adrenal
- originates from mesoderm
- consists of 3 layers: outer: zona glomerulosa; middle: zona fasciculata; inner: zona
reticularis
- Medulla
- originates from the neural crest
- develops in parallel with the sympathetic nervous system
- sympathetic nerves synapse directly with medullary cells, forming an interface between the
nervous system and endocrine system
- Adrenal Steroid Hormones
- Aldosterone
- produced by the zona glomerulosa
- released in response to angiotensin II and hyperkalemia
- low sodium delivery to the distal convoluted tubule in the kidney causes renin release from
the juxtaglomerular apparatus
- renin cleaves angiotensinogen into angiotensin I
- angiotensin I in converted into angiotensin II in the lung
- aldosterone causes salt and water absorption in the distal tubule, resulting in volume
expansion
- potassium and hydrogen ion are secreted into the urine
- Cortisol
- CRH secreted by the hypothalamus causes ACTH release from the anterior pituitary
- ACTH binds to receptors located in the zona fasciculata, resulting in the release of cortisol
- net effect of cortisol is to raise blood glucose concentrations
- also has potent anti-inflammatory, immunosuppressive, and metabolic effects
- Sex Steroids
- several weak androgens - androstenedione, DHEA - are produced in the zona reticularis
Adrenal Cortical Tumors
- Primary Hyperaldosteronism

- Clinical Manifestations
- accounts for 1% of all cases of hypertension
- Conn’s syndrome: hypertension, hypokalemia, polyuria
- hypertension often requires multiple medications to control
- hypokalemia may result leading to muscle weakness, cramps, or paresthesias
- may result from a solitary adenoma or bilateral adrenal hyperplasia
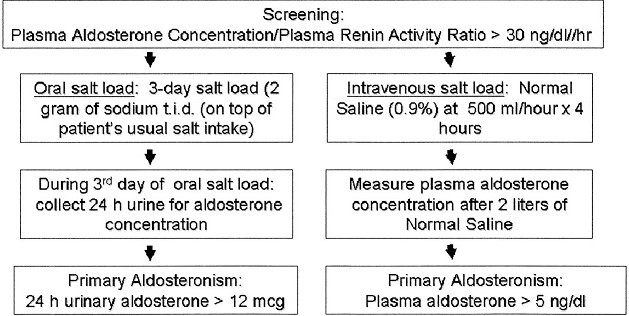
- Diagnosis
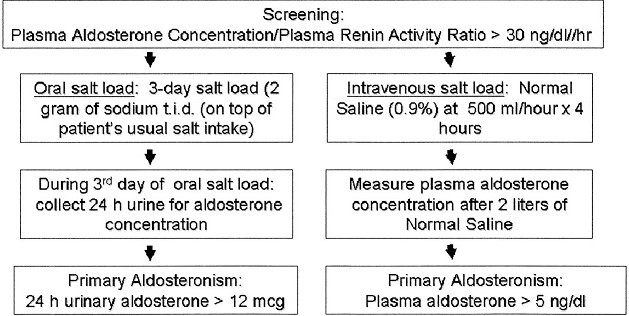
- Biochemical Screening
- should be performed in patients with hypertension and unexplained hypokalemia,
or in patients requiring multiple antihypertensive agents
- initial study is to determine the plasma aldosterone (PAC) to plasma renin (PRA) ratio
- PAC:PRA ratio > 20 is abnormal and mandates confirmatory testing
- inappropriately high aldosterone levels (nonsuppressible) after oral or IV salt
loading confirms the diagnosis
- Localization
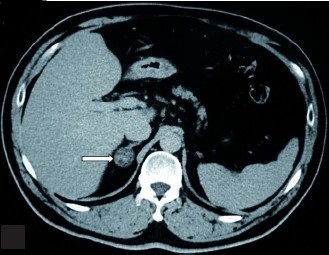
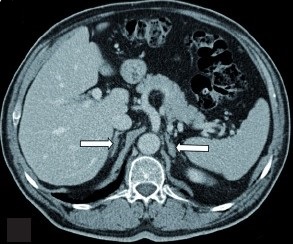
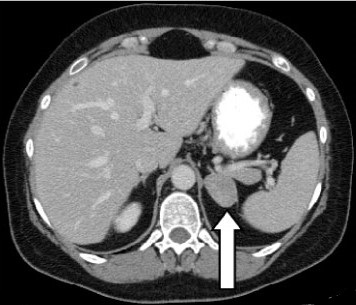
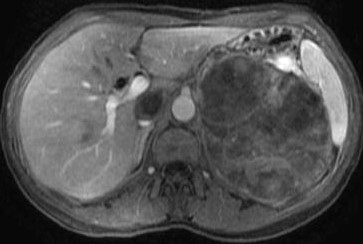
- CT Scan
- most lesions are less than 15 mm in size, making them difficult to image
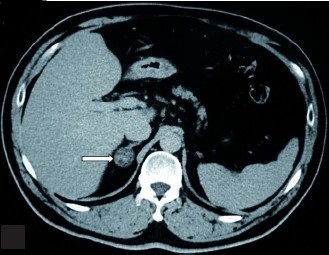
- if CT does not localize a lesion, or if bilateral nodules or adrenal
hypertrophy are seen, then selective adrenal vein sampling is required
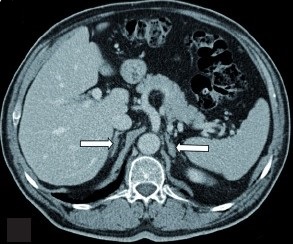 Bilateral Adrenal Hyperplasia
Bilateral Adrenal Hyperplasia
- Selective Adrenal Vein Sampling (AVS)
- requires simultaneous measurement of cortisol and aldosterone levels in the
IVC and right and left adrenal veins
- successful cannulation of an adrenal vein is confirmed by measuring a
fivefold increase in cortisol relative to the IVC (positive control)
- aldosterone/cortisol ratios for each adrenal vein are compared
- a positive test requires an aldosterone/cortisol ratio > 4 on one side
- AVS has a relatively low success rate, with the major difficulty being in
cannulating the right adrenal vein
- Treatment
- Laparoscopic Adrenalectomy
- indicated for a localized aldosteronoma
- spironolactone is used to optimize blood pressure before surgery
- potassium level should also be corrected before surgery
- 80% of patients will have normalization of blood pressure or a significant reduction
in blood pressure medication requirement
- Medical Therapy
- surgery is contraindicated for bilateral adrenal hyperplasia
- spironolactone is the preferred medical therapy
- Cushing’s Syndrome
- Clinical Manifestations
- syndrome of chronic glucocorticoid excess: hypertension, hyperglycemia, truncal obesity,
moon facies, easy bruising, muscle atrophy
- most common etiology is iatrogenic administration
- non-iatrogenic etiologies include pituitary adenoma (Cushing’s disease – 75%), adrenal
adenoma (15%), and ectopic ACTH production (NSCLC – 10%)
- Diagnosis
- Biochemical Screening
- 24-hour urine free cortisol test is the most sensitive and specific for
Cushing’s syndrome
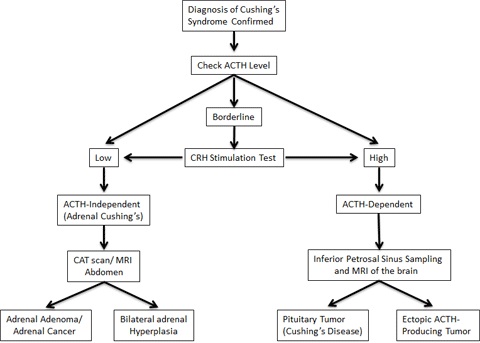
- after Cushing’s syndrome is confirmed, then measuring ACTH is necessary to determine
the specific cause – pituitary vs adrenal or ectopic
- adrenal disease will have very low or undetectable ACTH; high levels suggest a pituitary adenoma
or ectopic production
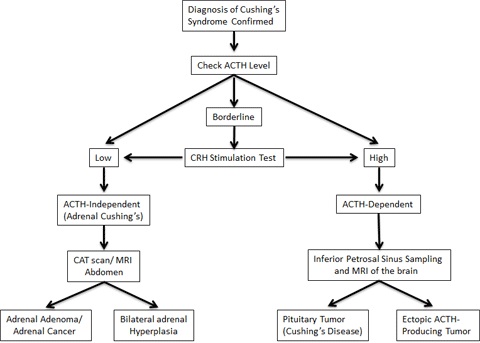
- Localization
- CT scan can visualize most solitary adrenal adenomas
- CT scan can also detect adrenocortical carcinoma or bilateral nodular hyperplasia
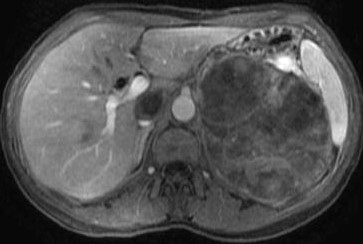
 Bilateral Nodular Hyperplasia
Bilateral Nodular Hyperplasia
- Treatment
- Surgery
- laparoscopic adrenalectomy is preferred
- metyrapone or ketoconazole can be used to control cortisol excess preop
- exercise and a high-protein diet should be encouraged to counteract preexisting muscle atrophy
- perioperative stress doses of hydrocortisone should be given
- contralateral adrenal may remain suppressed for several weeks, so perioperative
steroids will have to be gradually tapered
- 90% success rate, but resolution of symptoms may take months or years
- Medical Therapy
- reserved for cases of bilateral nodular hyperplasia
- bilateral adrenalectomy is a last resort for patients who fail medical management
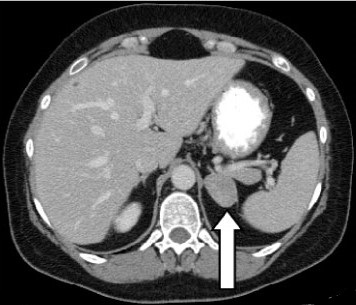
- Adrenocortical Carcinoma
- Epidemiology
- rare tumor
- annual incidence of 1/million population
- most patients are between ages 40 – 50
- also occurs in children < 5 years
- Clinical Manifestations
- 60% of patients have symptoms of hormone excess – Cushing’s syndrome, Cushing’s syndrome
and virilization, virilization alone (rare)
- mean tumor size is 9 – 13 cm
- local invasion is the rule: left adrenal cancers may invade the kidney, pancreas, spleen,
diaphragm; right tumors may invade the liver or IVC
- 40% of patients present with metastatic disease: lung, liver, peritoneum, bone
- CT scan typically shows a large heterogenous mass with irregular borders, central necrosis,
and local invasion
- Treatment
- radical surgery with en bloc resection of involved organs or lymph nodes is the only chance
for cure
- IVC invasion can be managed with resection/thrombectomy, and may require cardiopulmonary bypass
- adjuvant mitotane improves recurrence-free and overall survival in resected patients
- adjuvant XRT may benefit patients with positive resection margins or stage III disease
- Adrenal Metastases
- Clinical Features
- common site of metastasis because of the adrenal gland’s extensive blood supply
- most common primary cancers include lung, GI tract, breast, kidney, melanoma
- usually bilateral
- most often associated with other sites of metastatic disease
- adrenalectomy in the rare patient with an isolated adrenal metastasis can be associated with
long term survival

References
- Sabiston, 20th ed., pgs 963 – 986
- Cameron, 13th ed., pgs 741 - 749