Anesthetic Agents
- General Anesthesia
- elements of general anesthesia include unconsciousness with amnesia, analgesia, and muscle relaxation
- usually produced by a combination of IV and inhaled drugs
- IV induction agents are used to initiate anesthesia
- anesthesia is maintained by inhalational agents supplemented with IV opioids and muscle relaxants
- IV Induction Agents
- Propofol
- short half-life, lack of accumulation allows for rapid emergence from anesthesia
with no nausea
- side effects include hypotension, respiratory depression, pain on injection, and rare anaphylactic reactions
- must be used in caution with patients who are hypovolemic or who have CAD
- Etomidate
- rapid onset and offset of consciousness
- minimal cardiovascular effects, making it valuable in patients with CAD or hypovolemia
- side effects include a high incidence of post-op nausea, pain during injection, and transient
adrenocortical suppression
- Midazolam (Versed)
- reduces anxiety and produces amnesia
- usually administered in the immediate preoperative period
- may cause severe hypotension in hemodynamically unstable or hypovolemic patients
- effects of midazolam can be reversed by flumazenil
- Ketamine
- only induction agent that increases blood pressure and heart rate, making it useful in hypotensive patients
- has potent analgesic properties
- is a bronchodilator, making it useful in patients with asthma
- may cause delirium or hallucinations
- increases myocardial oxygen demand
- causes copious oropharyngeal secretions
- Inhalational Agents
- used as maintenance agents in adults
- at high doses, all agents can provide unconsciousness, analgesia, and muscle relaxation
- since at high doses the side effects are unacceptable, IV opioids and muscle relaxants are
used as supplemental agents, allowing for a lower dose of the inhalational agent
- Volatile Liquids
- isoflurane, sevoflurane, desflurane, and halothane are the most commonly used agents
- cause depression of cardiac contractility and stroke volume, resulting in dose-dependent hypotension
- triggering agents for malignant hyperthermia
- Nitrous Oxide
- rapid onset and offset
- reliably produces amnesic and analgesic effects
- may be combined with a volatile agent to permit a lower dose of the volatile agent
- has minimal cardiovascular effects
- associated with increased intracranial pressure
- causes expansion of gas-filled cavities, and is contraindicated in patients with
small bowel obstruction or pneumothorax
- Analgesia
- Opioids
- morphine, hydromorphone, fentanyl, sufentanil
- act on CNS μ-receptors
- not reliable hypnotic or amnesic agents
- cause minimal cardiac depression
- respiratory depression, sedation, itching, post-op nausea, and constipation are major disadvantages
- Naloxone is used to reverse the side effects of opioid overdose
- Ketorolac (Toradol)
- IV NSAID
- COX-1 and COX-2 inhibitor
- reduces prostaglandin synthesis
- major side effects include gastric bleeding, platelet dysfunction, kidney and
liver damage
- IV Tylenol
- reduces the amount of opioids required
- Neuromuscular Blocking Agents
- Depolarizing Agents
- succinylcholine
- mimics acetylcholine and keeps the post-synaptic membrane depolarized, resulting
first in contractions (fasciculations) and then decreased muscle excitability
- fast onset (< 60 seconds) and brief duration of action (5 – 8 minutes)
- used primary during rapid endotracheal intubation
- cannot be pharmacologically reversed
- side effects include bradycardia, hyperkalemia, and triggering of malignant
hyperthermia
- should not be used in burn or trauma patients
- Nondepolarizing Agents
- acetylcholine receptor antagonists – pancuronium, vecuronium, rocuronium
- peripheral nerve stimulator is required to gauge the depth and reversal of muscle
relaxation
- can be reversed by anticholinesterase drugs (neostigmine, edrophonium)
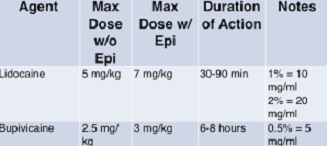
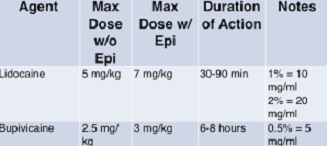
- Local Anesthetics
- Agents
- amides: lidocaine, bupivacaine, mepivacaine
- esters: cocaine, procaine, tetracaine
- all agents reversibly block nerve conduction by stabilizing sodium channels in their closed
states
- lidocaine has a more rapid onset and shorter duration of action than bupivacaine
- all agents are largely ineffective in acidic (inflamed) fields
- Toxicities
- toxic dose of lidocaine is 5 mg/kg
- toxic dose of bupivacaine is 3 mg/kg
- 1% lidocaine solution = 10 mg/mL
- for a 75 kg person, the toxic dose of lidocaine equals (75 kg x 5 mg/kg) / 10 mg/mL = 37.5 mL
- CNS Toxicity
- early symptoms include restlessness and tinnitus
- slurred speech, seizures, unconsciousness follow
- Cardiovascular Toxicity
- hypotension, increased P-R intervals, bradycardia, cardiac arrest may occur
- bupivacaine is more cardiotoxic than lidocaine
- Additives
- epinephrine increases the duration of action and slows absorption of the local anesthetic
- epinephrine-containing agents should not be injected into fingers or toes, because
vasoconstriction can lead to loss of a digit
- Regional Anesthesia
- avoids the complications of general anesthesia and airway manipulation
- sedation must be provided by IV administration of other drugs
- Spinal Anesthesia
- local anesthetic is injected directly into the dural sac surrounding the spinal cord,
usually as a single bolus injection
- the level of injection is below L1 – L2, where the spinal cord ends in most adults
- useful for inguinal hernia repair or lower extremity procedures
- the block causes loss of sensory, motor, and sympathetic function
- complications include hypotension from vasodilation, high spinal block leading to respiratory
compromise, spinal headache, urinary retention
- Epidural Anesthesia
- a catheter is inserted into the epidural space, such that repeated dosings are possible
- catheter may be left in place for several days to provide post-op analgesia
- particularly valuable in thoracic and vascular surgery
- may be associated with less post-op ileus and earlier ambulation in abdominal surgery
patients
- to avoid spinal hematomas, strict protocols regarding the timing of placement and removal of
catheters in patient receiving anticoagulants (LMWH) must be followed
- Peripheral Nerve Blocks
- local anesthetic can be injected peripherally adjacent to a large nerve or plexus
- some common examples include ankle blocks, intercostal blocks for rib fractures, transversus
abdominal plane (TAP) block for abdominal incisions
- Conscious Sedation
- refers to sedation administered for procedures done outside the OR by non-anesthesia personnel
- drugs used include an opioid for pain, often combined with an anxiolytic such as Versed
- an induction agent such as propofol may also be used for this purpose
- there is a narrow margin of safety between minimal sedation, which may be inadequate for the
procedure, and deep sedation, which may result in cardiovascular or respiratory depression
- major complications are hypoventilation and hypoxemia
- Joint Commission rules require that patients be managed and monitored as if they were in the OR with
an anesthesiologist present
- a monitoring assistant must be present who has no other responsibility during the procedure except
monitoring
- airway and resuscitation equipment must be present
- patients must be continuously monitored until the sedation has worn off
- physicians who provide conscious sedation must be appropriately credentialled
- office procedures need to follow the same precautions as practiced in the hospital
Pain control
- Patient-Controlled Anesthesia (PCA)
- increases patient control and autonomy
- opioids are the preferred agent for IV PCA
- patients receive prompt analgesia, receive smaller doses at more frequent intervals, and have a
lower incidence of drug-related side effects
- patients must have the mental and physical capacity to operate the device
- physicians must specify the loading dose, bolus dose, continuous infusion rate (basal rate),
lockout interval, and dose limits (1 hour max dose)
- the use of a basal rate is potentially dangerous, because drug is continuously delivered regardless
of demand, and may lead to respiratory depression
- Multimodal Anesthesia
- goal is to reduce opioid use and their attendant side effects and potential for addiction
- opioid-sparing drugs for post-op pain include IV tylenol, NSAIDS, steroids, anticonvulsants
(gabapentin)
- the best mixture of drugs has not been defined
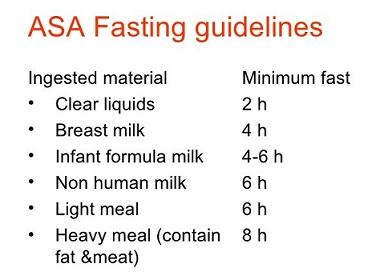
Preoperative Preparation
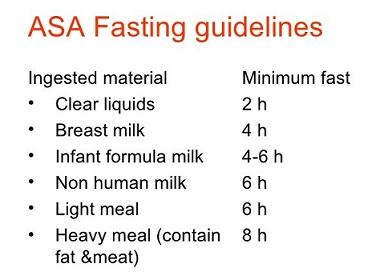
- Preoperative Fasting (NPO)
- goal is to prevent aspiration
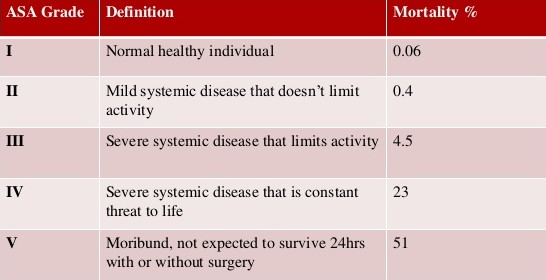
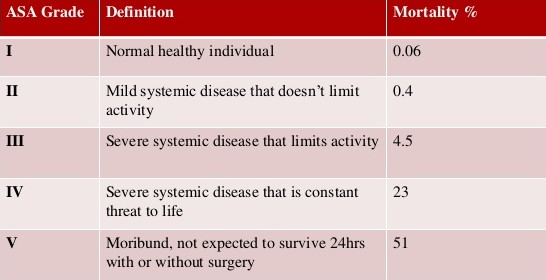
- Assessment of Physical Status
- American Society of Anesthesiologists (ASA) physical status classification system stratifies overall
perioperative risk of morbidity and mortality
- classified according to the degree to which underlying medical conditions produce functional limitations
Malignant Hyperthermia
- Pathophysiology
- hereditary autosomal dominant, life-threatening, hypermetabolic disorder of skeletal muscle
- a genetic defect in the ryanodine receptor leads to an uncontrolled rise of myoplasmic calcium, resulting in muscle activation
- triggering agents include all of the inhalation anesthetics (except nitrous oxide) as well as succinylcholine
- Clinical Manifestations
- fever
- increased metabolic rate (increased CO2 production, increased oxygen consumption, acidosis)
- increased sympathetic activity (tachycardia, hypertension, arrhythmias)
- muscle damage (muscle spasm, hyperkalemia, rhabdomyolysis)
- Emergency Management
- discontinue all triggering agents
- hyperventilation with 100% oxygen
- cool the patient
- Dantrolene is a specific antidote
- bicarbonate for acidosis
- calcium, glucose, insulin for hyperkalemia
References
- Schwartz, 10th
- Sabiston, 20th
- UpToDate. Overview of Anesthesia. Scott A. Falk, MD, Lee A. Fleisher, MD. March 16, 2020. Pgs 1 – 39