Anal Anatomy
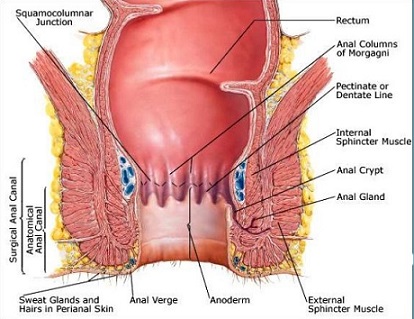
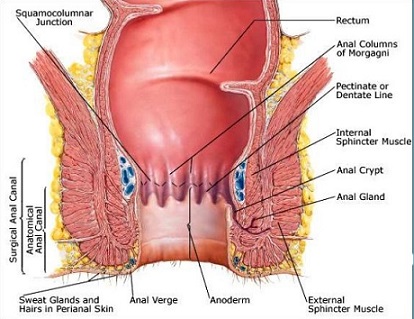
- Anal Canal
- anal verge is the junction between the anoderm and perianal skin
- dentate line is the mucocutaneous junction located 4 cm above the anal verge
- mucosa distal to the dentate line is a modified squamous epithelium devoid of hair and glands
- mucosa proximal to the dentate line is columnar epithelium
- the change between the 2 types of mucosa is not abrupt; there is a transitional zone that extends
for a variable length, from ~ 6 mm below to 20 mm above the dentate line
- anatomic anal canal extends from the anal verge to the dentate line
- surgical anal canal extends from the anal verge to the anorectal ring
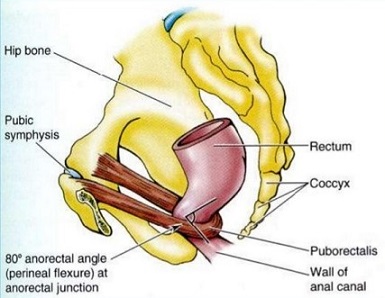
- anorectal ring is the lower border of the puborectalis muscle that is palpable on rectal exam –
located 1.0 to 1.5 cm above the dentate line
- posteriorly, the anal canal is attached to the coccyx by the anococcygeal ligament
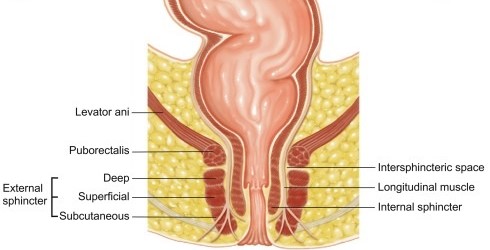
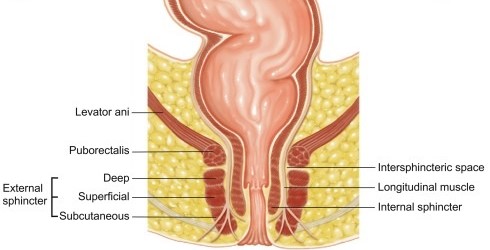
- Anal Sphincters
- Internal Sphincter
- continuation of the inner circular smooth muscle of the rectum
- involuntary muscle
- normally contracted at rest
- provides 80% of anal resting pressure
- major reflex response to rectal distention is relaxation
- External Sphincter
- voluntary muscle
- commonly divided into 3 parts: subcutaneous, superficial, and deep
- specialized continuation of the puborectalis muscle
- normally contracted at rest
- provides 20% of anal resting pressure and 100% of generated squeeze pressure
- its major reflex response to stimuli (postural change, rectal distention, increased intra-abdominal pressure)
is further contraction
- maximum voluntary contraction can only be maintained for 60 seconds before fatigue sets in
- Anal Glands
- body of the anal glands reside in the intersphincteric plane
- ducts of the glands penetrate the internal sphincter and terminate in the anal crypts
- anal crypts are located at the distal end of the columns of Morgagni, which consist of 8 to 14 mucosal folds
located above the dentate line
Anal Physiology
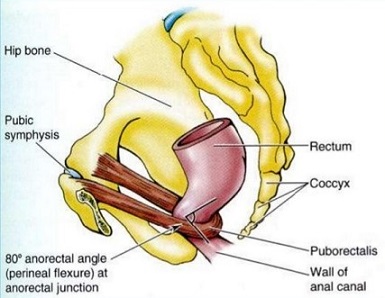
- Maintenance of Continence
- principal function of the anal canal is the maintenance of continence and the regulation of defecation
- principal mechanism that maintains continence is the pressure differential between the rectum (10 mm Hg) and the
anal canal (90 mm Hg)
- also, contraction of the puborectalis muscle maintains the anorectal angle at 80°, so that it
functions as a flap valve
- continence also requires an adequate rectal capacity with normal compliance
- Defecation
- as feces accumulate in the rectum, the rectal wall distends to accommodate the fecal mass
- as the rectum distends, the internal sphincter relaxes and the external sphincter contracts
- relaxation of the internal sphincter allows the rectal contents to reach the anal canal
- once in the anal canal, sensory receptors located within the anal canal or pelvic floor musculature determine the
nature of its contents – flatus, liquid, or solid stool
- if defecation is to proceed, the external sphincter must be voluntarily relaxed, which also straightens the anorectal angle
- a voluntary increase in intra-abdominal pressure moves the contents of the rectum into the anal canal
- with selective relaxation of part of the external sphincter, it is possible to selectively pass flatus but not stool
Rectal Prolapse

- Etiology
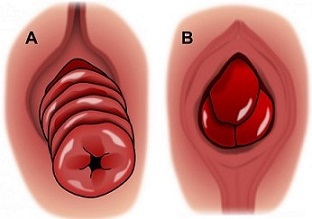
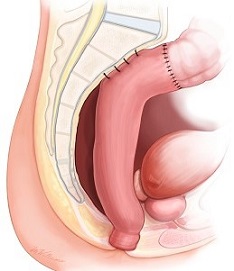
- complete prolapse is characterized by full-thickness eversion of the rectal wall through the anus
- partial prolapse involves prolapse of the mucosa only
- most commonly occurs in elderly women and institutionalized patients
- predisposing anatomic factors include a redundant rectosigmoid, deep pouch of Douglas, patulous anus,
diastasis of the levator ani, and lack of fixation of the rectum to the sacrum
- some studies suggest that intussusception is the primary cause, but what initiates the intussusception is not clear
- Clinical Manifestations
- a history of chronic constipation and straining is common
- most patients complain of the protrusion; in occult prolapse, a feeling of pressure and incomplete evacuation
may be the only symptoms
- many patients are incontinent
- chronically prolapsed mucosa may become ulcerated and cause significant bleeding
- digital rectal exam will usually reveal a patulous anus with poor sphincter tone
- a concomitant pelvic floor disorder (cystocele or prolapsed uterus) may also be present
- Diagnosis
- the best way to visualize the prolapse is to have the patient squat or sit on the toilet and strain
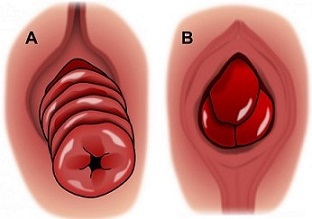
- seeing the concentric mucosal rings will help to differentiate prolapse from complicated hemorrhoidal problems
(radial folds)
- proctoscopy is mandatory and may demonstrate a polyp or cancer serving as the ‘lead point’ of the intussusception
- a complete colonoscopy or barium enema is necessary to rule out concomitant colon pathology
- anal manometry can document the degree of anal sphincter damage but does not influence the surgical procedure chosen
- defecography may help if the diagnosis is in question or if a concomitant pelvic floor disorder is suspected
- Surgical Options
- surgery is the mainstay of treatment
- can be managed from the perineal or abdominal approach
- the perineal approach is reserved for older patients who cannot tolerate a laparotomy
- abdominal procedures are associated with lower recurrence rates
- abdominal procedures can be done open or laparoscopically
- no ‘gold-standard’ procedure
- Narrowing of the Anus
- reserved for extremely high risk patients with incontinence
- prototypical procedure is the Thiersch-type anal encircling procedure using a synthetic mesh
- fecal impaction is the most common complication and laxatives and enemas are usually necessary postop
- wound infection and erosion of the mesh are also common
- procedure is rarely done now because of the high recurrence and complication rates
- Abdominal Procedures
- associated with lower recurrence rates than perineal procedures
- consists of rectal mobilization, ± sigmoidectomy, and rectal fixation
- Anterior Resection with Rectopexy
- major advantage is resection of the redundant sigmoid colon, which will improve constipation
- also, the rectum becomes fixed and adherent to the sacral hollow, helping to reduce recurrence
- major risk is anastomotic leak
- most surgeons will suture the rectum to the presacral fascia as a way of ensuring rectal fixation
- some surgeons also obliterate the cul-de-sac by suturing the endopelvic fascia anteriorly to the rectum
- both constipation and incontinence are improved by this procedure
- Rectal Fixation without Resection
- indicated when sigmoid resection is not required (no constipation)
- may be performed with sutures or mesh
- Suture Rectopexy
- the rectum is fully mobilized down to the levators and secured to the sacral fascia with
nonabsorbable sutures
- must avoid the presacral veins and nerves
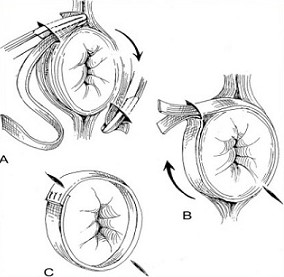
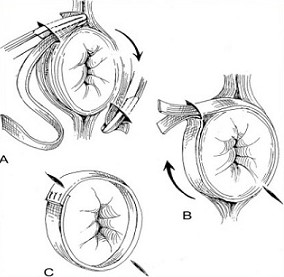
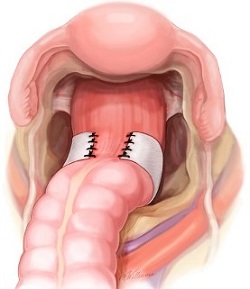
- Mesh Rectopexy
- the mesh is secured to the sacrum and then sutured to the rectum
- multiple options exist for fixing the mesh to the rectum
- obstruction and mesh erosion are complications
- Perineal Procedures
- usually reserved for patients who will not tolerate a laparotomy
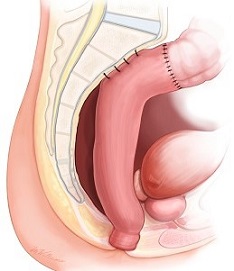
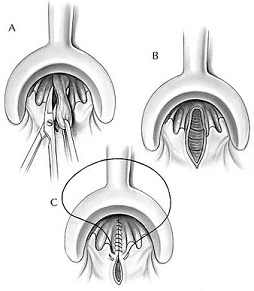
- Perineal Rectosigmoidectomy (Altemeier Procedure)
- for technical reasons, the length of the prolapse should be greater than 3 cm
- full-thickness circumferential incision is made in the prolapsed rectum 1 - 2 cm above
the dentate line
- cut edge of the rectum is pulled down and the mesorectum divided
- redundant rectum is then divided and an anastomosis is made to the anal ring
- the levator muscles may be plicated anteriorly for additional support
- recurrence rates appear to be high with this approach, probably because the rectum is
not fixed to the sacrum
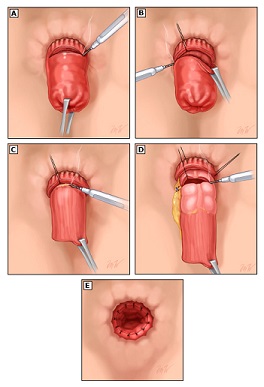
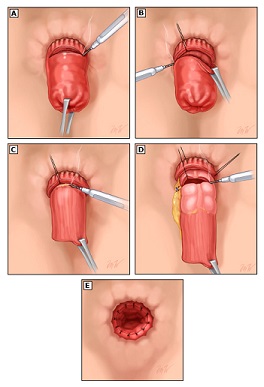
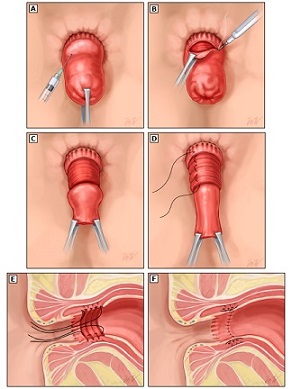
- Delorme Procedure
- reserved for patients with short prolapses
- not a full-thickness resection, but rather a resection of the redundant mucosa 1 – 2 cm proximal
to the dentate line
- the muscle layer is then plicated
- an anastomosis is then made between the mucosa at the level of the transection and the incision
proximal to the dentate line
- some surgeons will also plicate the levator muscles
Hemorrhoids
- Pathophysiology
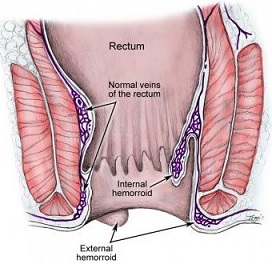
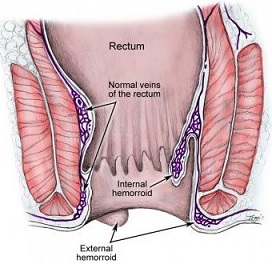
- Internal Hemorrhoids
- arise from specialized vascular and connective tissue cushions located in the left lateral, right anterior,
and right posterior positions in the anal canal
- consist of dilated arteriovenous channels (superior hemorrhoidal plexus) and connective tissue
- since they originate above the dentate line, internal hemorrhoids are covered by columnar mucosa which is
not sensitive to pain or touch
- by filling with blood during defecation, the cushions protect the anal canal from injury and aid in maintaining continence
- hemorrhoids refer to the abnormal enlargement of these cushions
- there are many theories as to what causes hemorrhoids: 1) downward displacement or prolapse caused by
straining, 2) destruction of the anchoring connective tissue system, 3) abnormal venous distention,
4) increased anal sphincter tone
- External Hemorrhoids
- originate below the dentate line and are covered by anoderm, which is very sensitive to pain
- arise from the inferior hemorrhoidal plexus
- since the superior and inferior hemorrhoidal plexuses communicate with each other, mixed hemorrhoids are common
- Clinical Manifestations
- Internal Hemorrhoids
- typically cause painless, bright red bleeding after defecation
- may also cause anal pruritis
- may also prolapse and become incarcerated
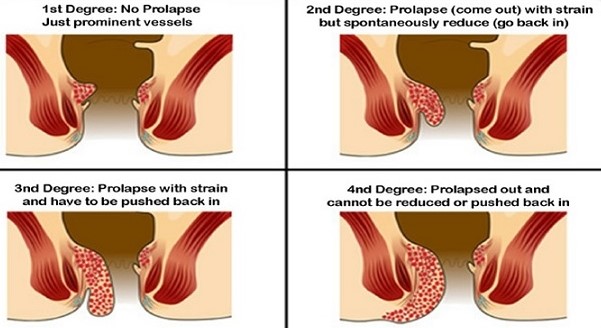
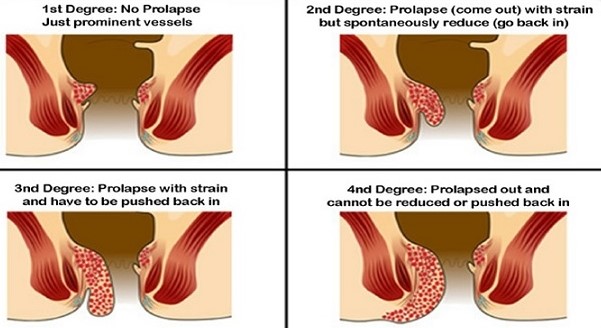
- Classification
- first degree: visible on anoscopy but do not prolapse below the dentate line
- second degree: prolapse out of the anal canal during defecation but spontaneously reduce
- third degree: require manual reduction
- fourth degree: incarcerated
- External Hemorrhoids
- may cause symptoms by swelling
- thrombosis may cause severe pain
- skin tags may form, which represent prior thrombosed hemorrhoids which have become organized into
fibrous appendages

- Diagnosis
- anoscopy is the definitive test
- consider screening colonoscopy if the patient is anemic, has risk factors for colon cancer or is due for
routine screening, or the hemorrhoidal disease is unimpressive
- Treatment
- Medical Therapy
- most patients with first- and second-degree hemorrhoids are adequately treated with bulking agents,
stool softeners, and increasing fluid intake
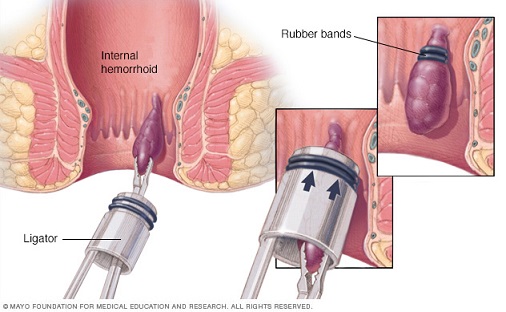
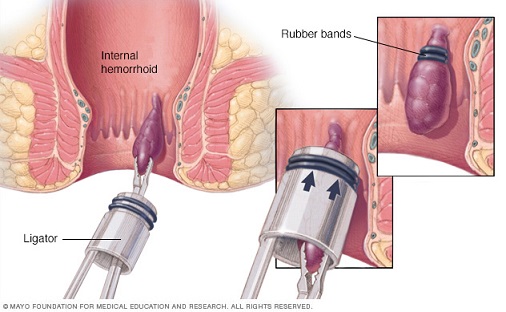
- Elastic Band Ligation
- effective treatment for most cases of second- and third-degree hemorrhoids
- can only be used on internal hemorrhoids – placement of elastic bands on anoderm or transitional epithelium is
extremely painful
- a single ligation may be done in the office every 2 weeks
- rarely, severe pelvic sepsis (pain, fever, difficulty voiding) has been reported after this procedure
- Sclerotherapy
- involves injection of a sclerosant (3% normal saline) into the internal hemorrhoid
- useful in patients who are on anticoagulants or who are immunocompromised or coagulopathic
- can treat all the hemorrhoids at one setting
- no need to stop the anticoagulants
- good short-term efficacy, but the recurrence rate is high
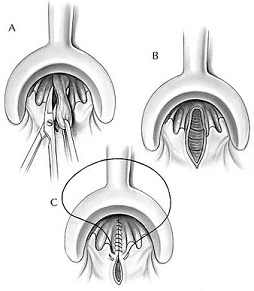
- Hemorrhoidectomy
- indications include large third-degree hemorrhoids, fourth-degree hemorrhoids, acutely thrombosed
hemorrhoids, gangrenous hemorrhoids
- may be done as an open or closed technique
- dissection must be superficial to the internal sphincter muscles
- a bridge of intact skin and mucosa should be left between excised hemorrhoid sites to avoid anal stenosis
- acutely thrombosed external hemorrhoids are best treated with excision not incision
- complications include urinary retention (30%), fecal incontinence (2%), infection (1%),
delayed hemorrhage (1%), and stricture (1%)
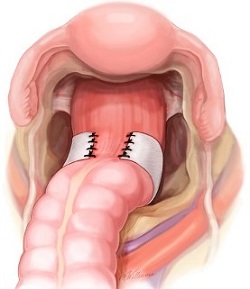
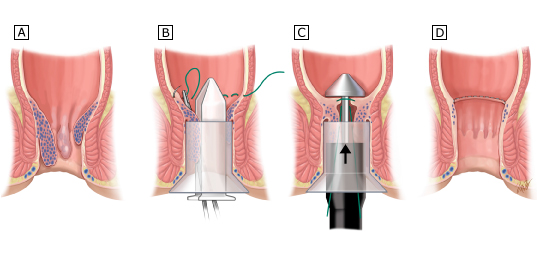
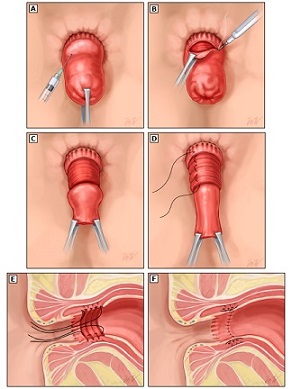
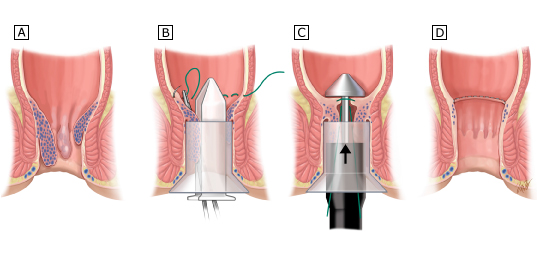
- Stapled Hemorrhoidopexy
- involves a circular resection and anastomosis of a 1- to 2-cm ring of anorectal mucosa and submucosa
- operation divides the vascular pedicles, resuspends the prolapsing tissue at the anorectal ring,
preserves the vascular cushions (important for continence), and avoids painful perianal wounds
- exact purse-string suture placement is crucial
- if the suture is placed too deep, then the vaginal wall may be incorporated anteriorly; if the suture is
placed too close to the dentate line, then severe intractable pain may result
- procedure is associated with higher patient satisfaction than conventional hemorrhoidectomy, but the
recurrence rates are also higher
- cannot be used for external hemorrhoids
- Special Problems
- Strangulated Hemorrhoids
- injection of dilute epinephrine together with 150 to 200 IU of hyaluronidase aids in reducing edema
and greatly facilitates the procedure
- must take care to preserve viable anoderm

- Pregnancy
- hemorrhoids often exacerbated in the 3rd trimester
- usual approach is conservative: Sitz baths, fiber, stool softeners
- often resolve spontaneously after delivery
- acutely thrombosed hemorrhoids can be operated on in the left lateral position
- Portal Hypertension
- anorectal varices are seen in 80% of patients with portal hypertension, but only account for 1% of massive
GI bleeding
- direct suture ligation may be tried
- TIPS procedure or portosystemic shunts may be required
References
- Sabiston 20th ed., pgs 1394 - 1402
- Cameron, 10th ed., pgs 190 - 194, 255 - 261
- UpToDate. Overview of Rectal Procidentia (Rectal Prolapse). Madhulika Varma, MD, Scott R. Steele, MD.
Mar 05, 2019. Pgs 1 – 22.
- UpToDate. Surgical Approach to Rectal Procidentia (Rectal Prolapse). Madhulika Varma, MD, Scott R. Steele, MD.
Sep 30, 2019. Pgs 1 – 38.
- UpToDate. Surgical Treatment of Hemorrhoidal Disease. David Rivadeneira, MD, Scott Steele, MD. Dec 03, 2019. Pgs 1 – 28.