Appendicitis
- Historical Aspects
- in the 1500s, a severe inflammation of the cecal region was known as ‘perityphlitis’
- first successful appendectomy was performed in 1735
- in 1886, Reginald Fitz accurately described the clinical history, physical findings, and pathology of
acute appendicitis and advocated early appendectomy as the appropriate treatment
- in 1889, McBurney reported on the importance of early operative intervention and described the point of
maximal tenderness (one-third of the distance between the anterior superior iliac spine and the umbilicus)
- Embryology and Anatomy
- arises from the cecum during the 8th week of gestation
- base of the appendix comes to lie medially near the ileocecal valve and is constant in location
- tip of the appendix may be found in many different positions (pelvic, retrocecal (60%), retroperitoneal)
- 3 taenia coli converge at the junction of the cecum and the appendix and can be a very useful landmark to
find the appendix
- has a separate mesoappendix with an artery and vein that are branches of the ileocolic vessels
- lymphatic drainage follows the ileocolic artery and drains into the mesenteric nodes
- Function
- immunologic organ and is a component of the gut-associated lymphoid tissue (GALT) system
- amount of lymphoid tissue peaks at puberty, stays steady for the next decade, and then decreases with age
- may serve as a reservoir of ‘good’ intestinal bacteria, and may aid in recolonization and maintenance of
normal colonic flora
- Incidence
- roughly parallels that of lymphoid development and peaks in the teen years
- more males than females (1.3:1)
- lifetime risk is 6% to 7%
- number of cases appears to be declining, for unclear reasons
- Pathophysiology
- luminal obstruction is the prime cause (fecalith, lymphoid hypertrophy, inspissated barium, seeds, tumors)
- normal mucous production rapidly leads to distention of the obstructed appendix
- as intraluminal pressure rises, capillaries and venules become occluded; eventually arteriolar pressure can
be exceeded, which leads to ischemia, infarction and perforation
- bacteria also multiply rapidly in the obstructed appendix and as mucosal blood supply becomes impaired, bacteria
are able to invade into the appendiceal wall, leading to transmural inflammation
- Clinical Manifestations and Diagnosis
- Symptoms
- anorexia is nearly always present and is often the first symptom
- appendiceal distention stimulates visceral afferent pain fibers, which produces a dull,
vague pain in the periumbilical region
- appendiceal distention may also stimulate peristalsis, so that abdominal cramping or an episode of
diarrhea may also occur
- as the inflammatory process progresses and involves the serosa and parietal peritoneum, the pain
becomes sharp and localizes to the right lower quadrant (somatic pain)
- most patients (75%) will have one or two episodes of vomiting, which usually occurs after the development of pain
- Signs
- physical findings are determined by the anatomic position of the appendix as well as whether it has ruptured
- Vital Signs
- temperature is rarely elevated more than 1° C in uncomplicated cases
- pulse is often normal unless rupture has occurred
- Position
- usually supine with thighs drawn up
- Physical Exam
- point tenderness is the principal physical finding
- point of maximal tenderness will vary depending on the location of the appendix
- extension of the hip (psoas sign) will elicit pain if the appendix lies on the psoas muscle
- flexion and internal rotation of the thigh (obturator sign) will elicit pain if the appendix lies
in the pelvis adjacent to the obturator internus muscle
- rectal examination is invaluable in diagnosing a pelvic appendicitis
- Rovsing’s sign – pain referred to the RLQ when the LLQ is palpated – also indicates the site of
peritoneal inflammation
- Lab Tests
- WBC Count
- most patients will have a WBC count between 10,000 and 18,000
- most patients with a WBC count < 10,000 will have a left shift
- however, it is possible to have acute appendicitis with a normal WBC count and differential
- nonsurgical problems such as gastroenteritis and ruptured ovarian cysts may also present with
an elevated WBC
- Urinalysis
- used to rule out a urinary source for the inflammation
- a few WBCs or RBCs may be present if the inflamed appendix overlies the ureter or bladder
- however, many WBCs, RBCs, or bacteria implicates the urinary tract
- Pregnancy Test
- mandatory in menstruating women
- Radiographic Studies
- not necessary in straight-forward cases (young males)
- Plain Films
- most useful in ruling out other diagnoses
- fecaliths are not commonly seen, but their presence is highly suggestive of appendicitis
- pneumoperitoneum is not seen in perforated appendicitis

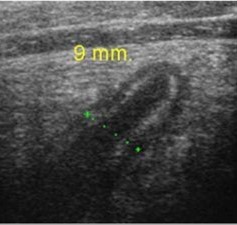
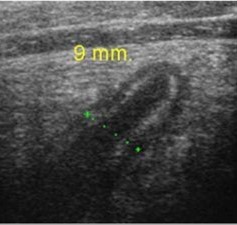
- Ultrasound
- appendix is identified as a blind-ending, non-peristaltic bowel loop originating from the cecum
- scan is considered positive if a non-compressible appendix 6 mm in diameter or greater is seen
- an easily compressible appendix 5 mm or less in diameter excludes appendicitis
- study is inconclusive if the appendix cannot be visualized
- results are very user dependent
- advantages include speed, no ionizing radiation, low cost
- used most often in pediatric and pregnant patients (to avoid radiation)
- most studies report sensitivities and specificities of 80% to 90%
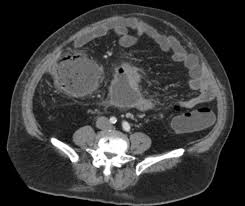
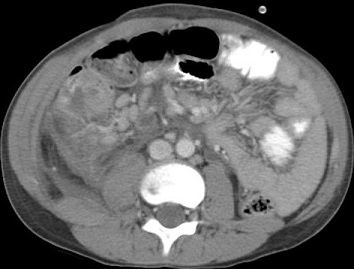
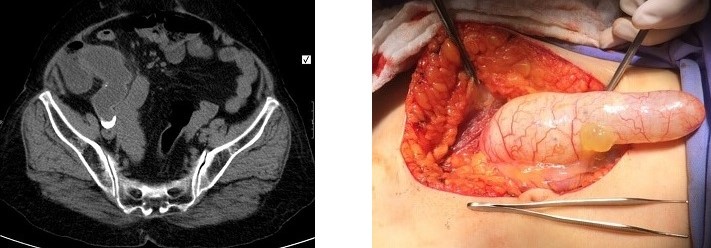
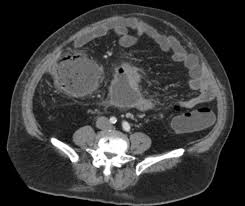
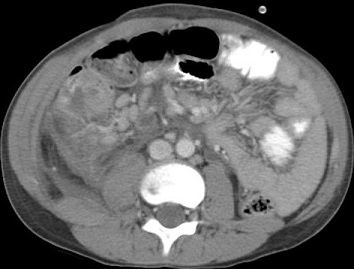
- CT Scan
- more sensitive and specific than ultrasound, but is more expensive and uses ionizing radiation
- useful in patients in whom physical examination is impossible or misleading (neurologically impaired,
immunosuppressed, morbidly obese)
- also helpful when an abscess is suspected to ascertain the feasibility of percutaneous drainage
- classic findings include an enlarged appendix (>6 mm) with surrounding inflammation (stranding)
- early appendicitis may not have CT findings

- MRI
- useful in pregnant patients (no contrast)
- sensitivity and specificity approaches 100%
- disadvantages include cost and limited availability after hours

- Differential Diagnosis
- Mesenteric Adenitis
- disease most commonly confused with acute appendicitis in children
- an upper respiratory infection is usually present or has just subsided
- Gastroenteritis
- nausea, vomiting, and diarrhea are usually much more prominent than in typical appendicitis
- abdominal pain is often cramping in nature
- Acute Ileitis
- cannot be distinguished from appendicitis on clinic grounds
- need to distinguish acute ileitis from Crohn’s disease at operation
- if the cecum is not involved, then an appendectomy is indicated
- Pyelonephritis
- may mimic a retrocecal appendicitis
- high fever, chills, right CVA tenderness, and many WBCs and bacteria in the urine usually
differentiates the two conditions
- Ureteral Stone
- pain is usually extremely severe and often referred to the labia or scrotum
- hematuria may be present; WBC count usually normal
- Pelvic Inflammatory Disease
- may mimic appendicitis if it is confined to the right tube
- pain and tenderness is usually lower
- may have exquisite cervical motion tenderness
- purulent vaginal discharge is often present
- Other Gynecologic Disorders
- ruptured follicle, ruptured or twisted ovarian cyst, endometriosis, and ruptured ectopic pregnancy
may all mimic acute appendicitis
- women between the ages of 15 and 45 historically have had the highest incidence of negative appendectomies (32% to 45%)
- Special Presentations
- Appendicitis in the Young
- diagnosis is often delayed because of the inability of the child to give an accurate history, and the
frequency of gastrointestinal complaints in this age group
- 20% incidence of ruptured appendices in the pediatric age group; children under 8 have twice
the perforation rate as older children
- appendicitis is very uncommon in children < 2 years old
- Appendicitis in the elderly
- morbidity and mortality rates of appendicitis are significantly increased in this population
- failure to consider the diagnosis, a more rapid progression to perforation, and coexisting disease
are all significant factors in this increased complication rate
- symptoms are often subtler and less typical than in younger patients
- CT scanning is important to rule out other pathologies that can mimic appendicitis (diverticulitis, colon cancer)
- Appendicitis during Pregnancy
- most common nonobstetric emergency (1 in 1500 pregnancies)
- equal distribution in all 3 trimesters
- as gestation progresses, the appendix becomes displaced laterally and superiorly, making the
diagnosis more difficult
- leukocytosis during pregnancy is physiologic, making lab evaluation less helpful
- US is usually the first diagnostic test; if inconclusive, then MRI, or rarely, CT scan can be used
- accurate diagnosis is crucial: negative appendectomy has a 4% fetal loss rate; uncomplicated appendicitis has a 2%
fetal loss rate; complicated appendicitis has a 6% fetal loss rate
- perforation is the factor most strongly associated with both maternal and fetal death
- diagnosis and surgical intervention should be rapid in the pregnant patient suspected of appendicitis
- controversial whether laparoscopic appendectomy has a higher fetal loss rate than open appendectomy
- Surgical Management
- Simple (Nonperforated) Appendicitis
- Operative Management
- safe, effective, and definitive treatment for appendicitis
- majority of surgeons and surgical societies consider appendectomy to be the standard or care
- the timing of the surgery remains controversial, but multiple studies have not shown an increased
perforation rate with a short in-hospital delay of 12 – 24 hours
- a single preoperative dose of an antibiotic that covers colon flora is usually adequate
- for patients on aspirin and/or Plavix, surgery does not need to be delayed
- Open Appendectomy
- done through a Rocky-Davis (transverse) or McBurney (oblique) right lower incision
- incision should be made over the point of maximal tenderness or a mass
- once the appendix is located, it must be delivered into the wound
- the mesoappendix is divided serially between clamps and ligated
- the base of the appendix is doubly ligated with absorbable suture
- it is traditional but not necessary to invert the appendiceal stump, unless the
viability of the appendix at the ligature site is questionable
- Laparoscopic Appendectomy
- safe and effective
- now the most common approach
- associated with improved cosmesis and a quicker return to normal activity
- lower incidence of wound infections, less pain, and shorter hospital stays
- higher incidence of intra-abdominal abscesses and longer operative times
- obese patients particularly benefit since they require larger incisions during open appendectomy
- conversion rate is ~ 10%
- Nonoperative Management
- some trials support antibiotic therapy alone for treatment of uncomplicated appendicitis
- 10% of patients will not respond to antibiotics and will require appendectomy during the
initial admission
- an additional 30% will develop recurrent appendicitis during the first year and require surgery
- in older patients, there is also a concern about missed neoplasms
- at present, appendectomy should still be considered the standard treatment
- Perforated Appendicitis
- occurs in up to 20% of patients with acute appendicitis
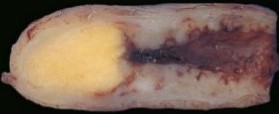
- may present with free perforation, an abscess, or with a phlegmon
- most patients treated nonoperatively initially will require an interval appendectomy
- Free Perforation
- patients may present with sepsis and generalized peritonitis
- hemodynamically unstable patients will require preoperative resuscitation
- once stabilized, patients will require an emergency laparotomy
- drains are not necessary unless a discrete abscess cavity is present
- Appendiceal Abscess
- many patients will initially be managed with a CT-guided abscess drainage and then
interval appendectomy 6 – 8 weeks later
- however, it is also reasonable to proceed with immediate appendectomy with operative
abscess drainage
- Appendiceal Phlegmon
- patients should initially be treated with antibiotics
- immediate operation is associated with injury to surrounding structures from dense
adhesions and inflammation
- patients who do not respond to nonoperative management will require rescue appendectomy (20%)
- Interval Appendectomy
- typically performed 6 – 8 weeks after hospital discharge
- the incidence of appendiceal neoplasms is much higher in interval appendectomy specimens (10% - 29%)
than in routine appendectomy specimens (~1%)
- interval appendectomy will also prevent episodes of recurrent appendicitis
- Management of the Normal Appendix
- with modern preoperative imaging, the negative appendectomy rate in the U.S. is 6%
- a noninflamed appendix should be removed at appendectomy because it removes appendicitis
from the differential diagnosis if the RLQ pain recurs
- the cecum, terminal ileum and mesentery should be inspected for acute and chronic inflammatory changes
- the distal 3 feet of ileum should be inspected for an inflamed Meckel’s diverticulum
- in women the uterus and both ovaries and tubes should be inspected
- if no pathology is found in the lower abdomen, then upper abdominal problems such as acute cholecystitis or
perforated peptic ulcer must be ruled out
- Complications
- Mortality
- mortality rate of unruptured appendicitis is 0.06%; mortality rate of ruptured appendicitis is 3% overall and 15% in the elderly
- death usually results from uncontrolled gram-negative sepsis
- Morbidity
- wound infection is common and is treated by opening the wound
- intraabdominal or pelvic abscesses may be treated by percutaneous drainage or transrectal drainage
References
- Schwartz, 10th ed., pgs 1241 - 1259
- Sabiston, 20th ed., pgs 1296 - 1311
- Cameron, 10th ed., pgs 252 – 255
- UpToDate. Management of Acute Appendicitis in Adults. Douglas Smink MD, MPH, David Soybel, MD. Apr 01, 2019. Pgs 1 – 38
- UpToDate. Well-Differentiated Neuroendocrine Tumors of the Appendix. Richard Swanson MD, Jennifer Ang Chan MD, MPH.
Dec 05, 2019. Pgs 1 – 35
- UpToDate. Nelya Melnitchouk, MD, MSc, FACS, Jeffrey Meyerhardt MD, MPH, Richard Swanson MD. Epithelial Tumors of the Appendix.
Nov 15, 2019. Pgs 1 – 67
- www.radiopaedia.org. Appendiceal Mucocele. Vikas Shah, MD