Locally Advanced Breast Cancer
Locally Advanced Breast Cancer
- Definition
- T3 lesions (> 5cm)
- T4 lesions – tumors involving the skin, chest wall, or inflammatory breast cancer
- N2 or N3 disease - bulky or fixed axillary adenopathy
- T3 Disease
- Neoadjuvant Chemotherapy
- in general, T3 tumors are too large for a cosmetically acceptable lumpectomy
- preoperative chemotherapy can result in a significant reduction in tumor size for 50% - 80% of patients,
often allowing them to avoid a mastectomy
- HER2-positive patients should also receive a HER2-targeted drug
- multiple studies demonstrate increased rates of breast conservation with the use of neoadjuvant therapy
- there is no survival advantage or detriment to neoadjuvant therapy, but clinical response does correlate
with survival
- since 10% - 15% of patients will have a complete response by clinical exam and imaging, a metallic clip
should be placed at the primary tumor site before beginning treatment
- Surgical Treatment
- clinical exam is usually sufficient to judge tumor response
- whether a patient is a candidate for breast conservation is dependent on the extent of tumor involvement
after completing neoadjuvant treatment
- patients who have a complete clinical response still require surgery
- patients whose disease progresses while getting neoadjuvant treatment should have surgery, rather than
switching to another chemotherapy regimen
- Management of the Axilla
- depends on whether the axilla was positive prior to treatment, and whether the patient had a SLN biopsy prior to treatment
- whether to perform the SLN biopsy before neoadjuvant treatment or after completion is unknown
- pretreatment SLN biopsy allows for accurate pretreatment staging
- posttreatment SLN biopsy provides nodal status information after treatment, which is the strongest
predictor of outcome
- there is a higher failure rate of lymphatic mapping after neoadjuvant treatment
- Clinically Negative Axilla Pretreatment
- No Pretreatment SLN Biopsy
- patient should have a posttreatment SLN biopsy
- Negative Pretreatment SLN Biopsy
- no further treatment of the axilla is required
- Positive Pretreatment SLN Biopsy
- patients will require axillary radiation or a completion axillary node dissection
- if a patient has one or two positive SLNs and will undergo breast conservation treatment,
then axillary radiation is reasonable
- if a patient will require mastectomy and has no indication for postmastectomy radiation,
then completion axillary node dissection is indicated
- Clinically Positive Axilla Pretreatment
- patients with grossly positive nodes (N2, N3) should undergo ALND at the time of definitive breast surgery
- management of biopsy-proven N1 disease will depend on the response to neoadjuvant treatment
- f the node remains clinically positive then an ALND should be done at the time of definitive breast surgery
- if the node becomes clinically negative, then a posttreatment SLN biopsy can be done
- Posttreatment SLN Biopsy
- if negative, then axillary radiation is sufficient
- if one or two positive SLNs, then axillary radiation is sufficient
- for three or more positive SLNs, then ALND is required
- T4 Disease
- includes tumors involving the chest wall, skin, ulceration, satellite skin nodules,
bulky or fixed axillary nodes, internal mammary or supraclavicular nodal involvement,
inflammatory breast cancer

- surgery alone provides poor local control
- current management includes surgery, radiation, and systemic chemotherapy, with the sequence determined
by the patient’s circumstances
- Inflammatory Breast Cancer (IBC)
- most aggressive subtype of breast cancer
- long-term survival rates are < 50%
- accounts for 0.5% - 2% of breast cancer cases
- results from diffuse tumor involvement of the dermal lymphatics
- Clinical Presentation
- has a rapid onset, with progression over several weeks to months
- presents with erythema, warmth, and swelling of at least one third of the breast
- may be confused with mastitis
- skin may have the classic peau d’orange appearance: edema and dimpling at sites of hair follicles
- there may or may not be a discrete mass on exam
- nipple changes such as retraction may be present
- palpable or matted axillary nodes are usually present

- Diagnosis
- mammographic findings may include an obvious tumor mass, a large area of calcifications,
skin thickening
- pathologic hallmark is a full-thickness skin biopsy that demonstrates cancer invading the dermal lymphatics
- however, IBC is a clinical diagnosis and can be made without pathologic confirmation of dermal lymphatic invasion
- if a lesion is identified in the breast, or if there are suspicious axillary nodes, then an
image-guided core biopsy should be done to confirm the diagnosis and to provide tissue for
ER, PR, and HER2 receptors
- Diagnostic Criteria
- all of the following must be met to make a diagnosis of IBC:
- rapid onset of breast erythema, edema and/or peu d’orange, and/or warm breast, with or without an underlying
palpable mass
- duration < 6 months
- erythema of > one-third of the breast
- pathologic diagnosis of breast cancer
- Staging Work Up
- at diagnosis, ~33% of patients will already have distant metastases
- CT of the chest, abdomen, pelvis
- bone scan
- breast MRI and PET scan are not routinely obtained
- Treatment
- Neoadjuvant Chemotherapy
- systemic chemotherapy is the cornerstone of treatment
- Trastuzumab is added for HER2-positive tumors
- clinical response to neoadjuvant chemotherapy can be a good indicator of prognosis
- Surgery
- modified radical mastectomy is the procedure of choice in patients who have had a good response to chemotherapy
- no role for breast conservation or skin-sparing mastectomies
- SLN biopsy is unreliable in patients with IBC
- reconstruction should be delayed until all treatments are finished
- palliative mastectomy may have a role in some patients who do not respond to chemotherapy
- Radiation
- used in a neoadjuvant role for patients who do not respond to chemotherapy
- following MRM, patients receive radiation to the chest wall, axilla, supraclavicular nodes,
and possibly the internal mammary nodes
- purpose is improved locoregional control – there is probably no effect on overall survival
- Hormonal Therapy
- most cases of IBC are ER- and PR-receptor negative
- tamoxifen or an aromatase inhibitor is valuable in the small subset of patients who are receptor-positive
Unusual Breast Tumors
- Paget’s Disease
- accounts for ~ 1% of breast cancer cases
- ~90% of patients have an underlying invasive or in situ breast cancer
- the invasive cancers tend to present at a more advanced stage and are often ER-negative;
their 5-year survival is ~ 40%
- Presentation
- characterized by nipple irritation and erythema
- may progress to crusting and ulceration
- may spread out onto the skin of the areola and breast
- differential includes dermatitis, eczema, postradiation dermatitis
- 50% of patients have a palpable breast mass
- 20% of patients have a mammographic abnormality without a palpable mass
- 25% of patients have an occult DCIS without a mass or mammographic abnormality
- diagnosis is made by a full thickness biopsy of the nipple
- any underlying mass or mammographic abnormality should be biopsied as well

- Pathology
- Paget cells (intraepithelial adenocarcinoma cells) do not originate in the skin of the nipple
- they spread into the lactiferous sinuses under the nipple and upward to invade the epidermis of the nipple
- Paget cells do not invade the dermal basement membrane and are characterized as carcinoma in situ
- Paget cells can resemble melanoma, and occasionally immunohistochemistry may be required to make the diagnosis
- Staging
- Paget’s disease does not change the stage of the underlying breast cancer
- if an invasive cancer or in situ cancer is not identified, then the stage is Tis (Paget)
- Treatment
- Management of the Breast with a Palpable Mass or Abnormal Mammogram
- the nipple-areolar complex and the underlying breast cancer must both be excised
- for the majority of patients, this will require a simple mastectomy with or without
immediate reconstruction
- in a few patients, breast conservation/XRT can be performed with an acceptable cosmetic result
and negative margins
- Management of the Breast when there is no Palpable Mass or Abnormal Mammogram
- most patients will have an occult DCIS or invasive cancer, making a simple mastectomy the
standard treatment option
- breast conservation with resection of the nipple-areolar complex and XRT is another acceptable option
- Management of the Axilla
- indications for SLN biopsy or ALND are the same as for any breast cancer
- for DCIS requiring mastectomy, a SLN biopsy should be done in case an invasive cancer is identified
on final pathology
- invasive cancers with a clinically-negative axilla require a SLN biopsy
- invasive cancers with a clinically-positive axilla require a confirmatory biopsy, and then an ALND
- Adjuvant Therapy
- systemic therapy will be guided by the standard indicators: tumor size, nodal status, receptor status
- Male Breast Cancer
- accounts for 0.8% of breast cancer cases (2100 cases/year)
- when matched for stage, survival is the same as for women
- Risk Factors
- radiation exposure
- estrogen and androgen imbalance: testicular disease, obesity, cirrhosis
- genetic risk factors include Klinefelter’s syndrome (47, XXY), BRCA2 mutations, family history
- Presentation
- most present with a breast mass
- major differential diagnosis is gynecomastia
- may also have axillary adenopathy or nipple retraction
- Diagnosis
- mammogram
- core needle biopsy
- Treatment
- depends on stage and local extent of the tumor
- breast conservation/radiation is possible if desired
- SLN biopsy is an effective staging procedure in men
- majority of patients are treated with mastectomy/SLN or modified radical mastectomy
- adjuvant hormonal therapy with tamoxifen or aromatase inhibitors is indicated for ER-positive disease
- systemic chemotherapy is used for patients at high risk of systemic disease
- Phyllodes Tumors
- account for < 1% of all breast neoplasms
- capable of a wide range of biologic behaviors, from benign to widely metastatic
- classified as benign, borderline, or malignant
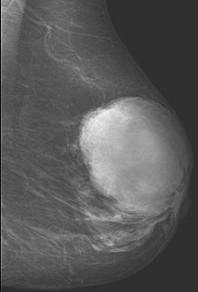
- Presentation
- most present as a smooth, well-defined multinodular mass that is mobile, painless, and fast-growing
- average tumor size is 4 – 7 cm
- 20% present as a nonpalpable mass identified on screening mammogram
- median age at presentation is 42 – 45 years
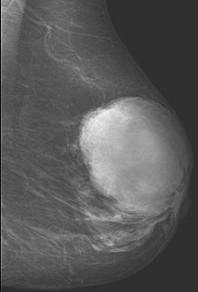
- Diagnosis
- core biopsy is preferred over FNA, and is usually diagnostic
- features that distinguish phyllodes tumors from fibroadenomas include increased cellularity,
mitosis, stromal overgrowth, and fragmentation
- if core biopsy is indeterminate, than an excisional biopsy will be necessary
- Treatment
- Surgery
- goal is a wide excision with 1 cm margins, especially for borderline or malignant tumors
- breast conservation is a reasonable option if adequate margins and an acceptable cosmetic outcome
can be obtained
- sentinel node biopsy is not necessary since lymph node involvement is very rare
- Radiation
- not indicated for benign tumors that have been widely excised
- recommended for borderline or malignant lesions following excision to reduce local recurrence rates
- Adjuvant Chemotherapy
- no role in benign and borderline tumors
- controversial whether it benefits patients with high-risk (>10 cm) malignant tumors
- hormonal therapy is not effective against phyllodes tumors
References
- Sabiston, 19th ed., pgs 863 – 867
- Cameron, 11th ed., pgs 595 – 599, 599 – 601, 618 – 621
- UpToDate. Overview of the Treatment of Newly Diagnosed, Non-metastatic Breast Cancer. Taghian MD, Alphonse. Aug 21, 2019. Pgs 1 - 30
- UpToDate. General Principles of Neoadjuvant Therapy for Breast Cancer. Sikov MD, William. May 16, 2019. Pgs 1 – 39
- UpToDate. Inflammatory Breast Cancer: Clinical Features and Treatment. Taghian MD, Alphonse. Sep 26, 2018. Pgs 1 – 23
- UpToDate. Paget Disease of the Breast. Sabel MD, Michael. Apr 03, 2018. Pgs 1 – 29
- UpToDate. Phyllodes Tumors of the Breast. Grau MD, Ana. May 09, 2019. Pgs 1 – 23