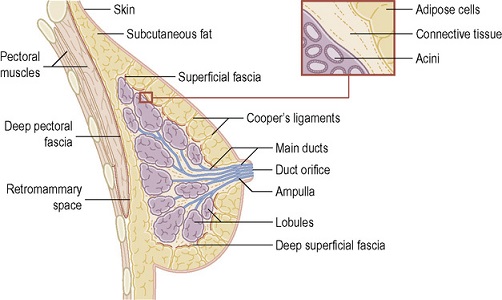
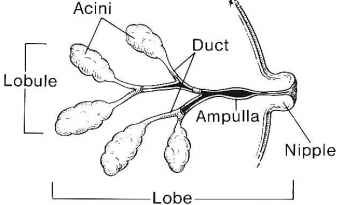
Anatomy and Physiology
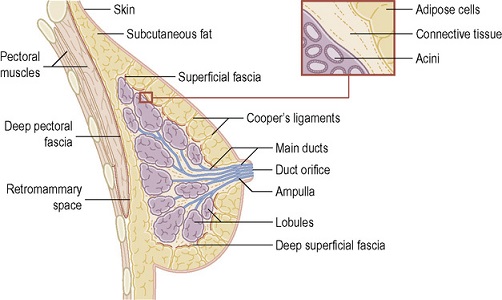
- Breast Anatomy
- Lies between the subdermal layer of adipose tissue and the deep pectoral fascia
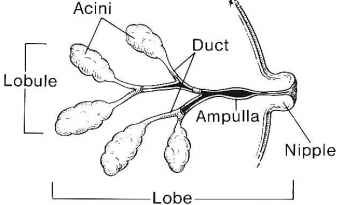
- Parenchyma is composed of 15 – 20 lobes that are in turn composed of multiple lobules
- Each lobe terminates in a major duct
- Each major duct has a dilated portion (lactiferous sinus) below the nipple-areolar complex
- No distinct investing fascia of the breast
- Cooper’s ligaments provide shape and support for the breast as they course from the skin to the underlying fascia
- Principal blood supply comes from perforating branches of the internal mammary and intercostal arteries
- Physiology
- Estrogen is responsible for duct development and proliferation
- Progesterone causes lobular development after ovulation
- If pregnancy does not occur, estrogen and progesterone levels decline, resulting in the onset of menstruation
Diagnosis of Breast Disease
- History
- Details of the specific breast complaint: history of mass, breast pain, nipple discharge, skin changes
- Reproductive history: age at menarche, age at menopause, pregnancies – including age at first pregnancy
- Previous history of breast biopsies, including pathology reports
- History of hormone replacement or OCP use
- Family history of breast or ovarian cancer, and the age at diagnosis
- Physical Exam
- Visual inspection for obvious masses, asymmetries, skin changes, dimpling
- Nipples: inspect for retraction, inversion, excoriation or rashes (Paget’s disease)
- Inflammatory changes: erythema, warmth, edema (peau d’orange)
- Breast palpation: masses are characterized by size, shape, consistency, location, and fixation to the skin
or musculature
- Axillary node palpation is best done with the patient sitting with her arm outstretched or on her hip
- Imaging
- Diagnostic Mammography
- Primary study to evaluate clinical findings
- 2 standard views: mediolateral oblique and craniocaudal
- Additional views may be necessary: magnification views to evaluate microcalcifications, compression
views for mass lesions
- Breast density limits mammogram sensitivity: 10% to 15% of clinical cancers may have a negative mammogram
- Digital mammography allows manipulation and enhancement of images to facilitate interpretation
- Computer-assisted diagnosis (CAD) increases sensitivity and specificity of mammography over radiologist
interpretation alone
- Suspicious findings on mammogram can usually be biopsied stereotactically
- Ultrasound
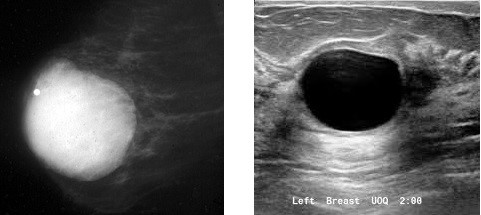
- Primary value is to determine whether a mammographic lesion is cystic or solid
- Not used as a primary screening modality
- Suspicious mass lesions may be biopsied under ultrasound guidance
Benign Breast Conditions
- Cysts
- Often present as a palpable abnormality or cause of breast pain
- On physical exam, they are usually smooth, round, firm, and tender
- Peak incidence is between 35 and 50 years of age
- Classified as simple, complicated, or complex
- Simple Cysts
- Simple cysts have thin walls and septa without a solid component
- Benign lesions with no risk of malignancy
- Small, asymptomatic simple cysts can be observed
- Palpable or symptomatic cysts can be aspirated under palpation or ultrasound guidance
- Only bloody cyst fluid needs to be sent for cytopathology
- Cysts that recur more than two times should be excised
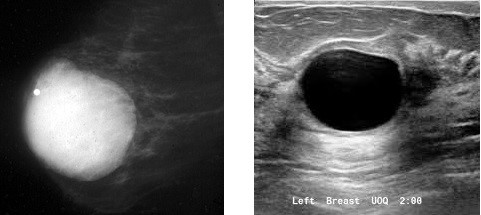
- Complicated Cysts
- Contain echogenic debris without solid components, thick walls, or thick septa
- Breast cancer risk is less than 1%
- Most are classified as BI-RADS 2, and are managed like simple cysts
- If the cyst is classified as BI-RADS 3, then the imaging should be repeated in 6 months, unless the
patient desires biopsy or excision
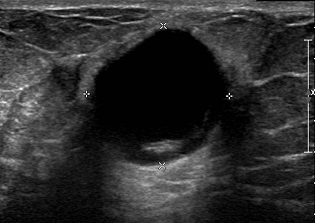
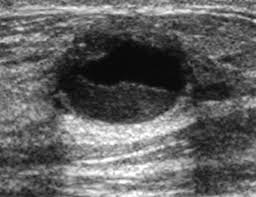 Complicated cyst with echogenic debris
Complicated cyst with echogenic debris
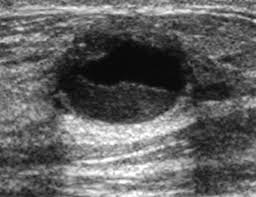
- Complex Cysts
- Contain both cystic and solid components, as well as thick walls and septa
- Usually classified as BI-RADS 4
- Require an image-guided core needle biopsy or a needle-localized excisional biopsy
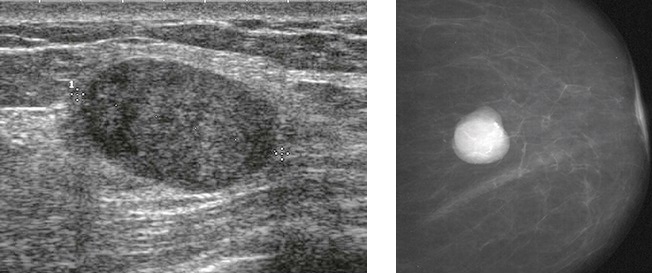
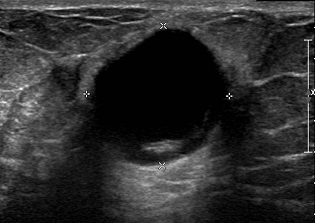 Complex cyst with a thick wall and mural nodule
Complex cyst with a thick wall and mural nodule
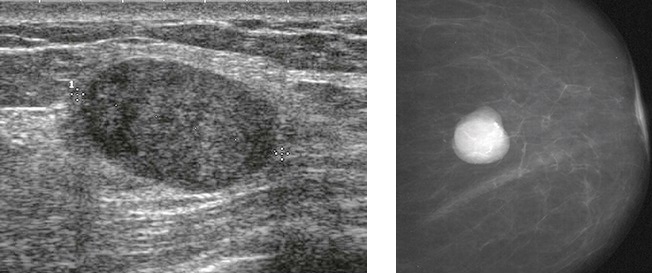
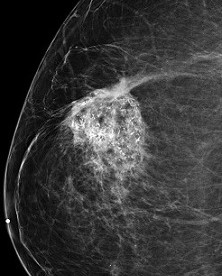
- Fibroadenoma
- Most common cause of a breast mass in women < 30
- Presents as a firm, round, smooth, rubbery, freely mobile mass
- Cannot be distinguished from cysts on mammogram
- Ultrasound shows a well-defined solid mass
- Neither a premalignant lesion nor a risk factor for breast cancer
- Excision is not mandatory, but it is often chosen to remove worry
- If a nonoperative approach is taken, then the diagnosis should be confirmed by a core-needle biopsy
- Rapid growth raises the suspicion of a phyllodes tumor, which cannot be distinguished from a fibroadenoma
on core biopsy
- Breast Pain
- Classified as cyclical or noncyclical
- Symptoms range from vague to debilitating pain
- Cyclical Pain
- Often called fibrocystic breast disease
- Hormonally driven, usually presenting the week before the onset of menses and dissipating
with the onset of menses
- May be associated with oral contraceptives or estrogen replacement therapy
- Symptoms are usually bilateral and diffuse and cease at menopause
- Patients may present with palpable lumps, which fluctuate in size and discomfort with the menstrual cycle
- Imaging is used selectively based on physical findings and whether the patient is up to date on screening
- Treatment
- Support bras and sports bras during exercise are often recommended
- Warm compresses or ice packs provide relief to some women
- Topical NSAIDS (Diclofenac) have been validated in clinical trials
- Eliminating caffeine, a low-fat diet, primrose oil, and vitamin E are often recommended,
but the evidence to support their efficacy is lacking
- Occasionally a short course of tamoxifen or danazol is necessary to relieve symptoms
- Often, the only treatment necessary is reassurance that breast pain is not a common symptom
of breast cancer
- Noncyclical Pain
- Not related to the menstrual cycle
- May be constant or intermittent, and is more likely to be unilateral
- Potential causes include cysts, fibroadenomas, or infections
- Extramammary causes include underlying bone disease, costochondritis, or fibromyalgia
- Treatment is directed to the underlying cause, if it can be identified
- Nipple Discharge
- Discharge that is bilateral and multiductal is a common benign physiologic process
- Discharge that is spontaneous, unilateral, recurrent, and involving a single duct is suspicious and
requires further investigation
- Suspicious Nipple Discharge
- May be clear, blood-tinged, or bloody
- Most common etiology is a papilloma
- DCIS or invasive cancer accounts for 5% - 15% of cases
- Increasing age is predictive of the risk of breast cancer in women with nipple discharge
- Bloody nipple discharge is associated with a higher risk of breast cancer than nonbloody discharge
- Paget’s disease, eczema, and local infections may mimic nipple discharge
- Breast Examination
- Observe for skin changes, symmetry, position of the nipples, skin retraction, dimpling,
and ulceration or crusting of the nipple
- Determine which quadrant and duct is responsible by applying clockwise pressure around the areola
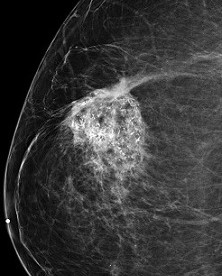
- Imaging
- Mammogram
- Should be obtained in all women ≥ 30 years old, although the sensitivity is low
- Ultrasound
- Most useful study
- Focus is on the periareolar area
- Provides good visualization of dilated ducts and any nodules inside them
- Facilitates core needle biopsy or wire localization for surgery
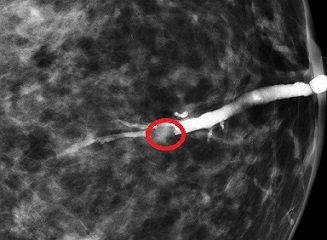
 Intraductal Papilloma
Intraductal Papilloma
- Ductography
- Technically challenging procedure that requires cannulation of the involved duct
- Valuable when ultrasound does not visualize the lesion
- Negative ductography does not exclude a cancer
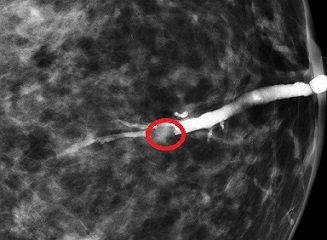
- Surgical Treatment
- Papillomas are managed with a terminal duct excision through a circumareolar incision
- After complete excision, 17% - 20% of papillomas are found to contain cancer
- DCIS or invasive cancers are managed with either a partial mastectomy or mastectomy
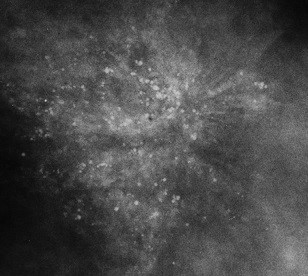
- Sclerosing Adenosis
- Mimics carcinoma both grossly and histologically
- Often contains microcalcifications which mimics DCIS
- Presents as a palpable mass or a suspicious finding on mammogram
- No significant malignant potential
- Excision is not required if the diagnosis is secure
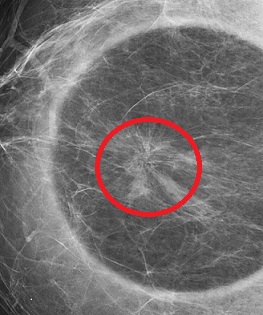
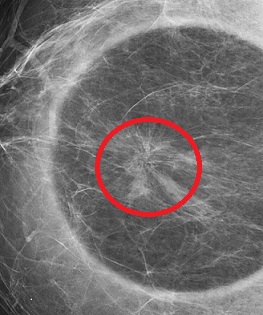
- Radial Scar
- Belongs to a group of lesions known as complex sclerosing lesions
- Mimics carcinoma both mammographically and on physical exam
- May present as a spiculated mass with skin dimpling
- Characterized pathologically by a central scar
- Usually requires excision to rule out an underlying carcinoma, which is found in 20% of cases
- Fat Necrosis
- Can mimic cancer by producing a palpable mass
- On mammogram, may present as a spiculated mass with microcalcifications
- May be preceded by a history of trauma, prior breast surgery (reduction), or radiation treatment
- Often requires surgical excision to confirm the diagnosis
- No malignant potential
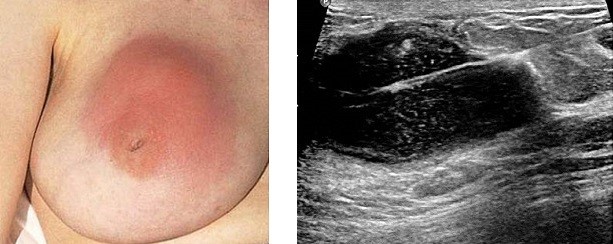
Breast Infections
- Mastitis
- Generalized cellulitis of the breast
- Presents with erythema, pain, and tenderness to palpation
- Often complicates lactation
- Streptococci and staphylococci are the most common offending organisms
- Differential diagnosis includes inflammatory carcinoma, which will not respond to antibiotic therapy

- Abscess
- S. aureus is the most common organism isolated
- Often occurs within several weeks of beginning lactation
- Ultrasound is used to aspirate free-flowing abscess cavities
- Treatment of multiloculated abscesses will require incision and drainage
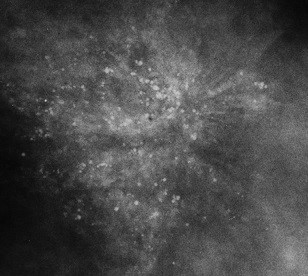
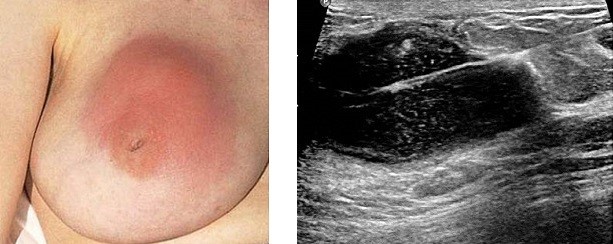 Ultrasound-guided drainage of a breast abscess
Ultrasound-guided drainage of a breast abscess
References
- Sabiston, 19th ed., pgs 824 – 840
- Cameron, 11th ed., pgs 565 – 567
- UpToDate. Overview of Benign Breast Disease. Sabel MD, Michael. Sept 19, 2018. Pgs 1 – 27
- UpToDate. Breast Cysts: Clinical Manifestations, Diagnosis, and Management. Laronga MD, Christine.
Aug 13, 2019. Pgs 1 – 18
- UpToDate. Breast Pain. Golshan MD, Mehra. May 15, 2018. Pgs 1 – 21
- UpToDate. Nipple Discharge. Golshan MD, Mehra. Feb 12, 2018. Pgs 1 – 24
- Ultrasound images from radiopaedia.org