Inflammatory Bowel Disease
Ulcerative Colitis
- Definition
- diffuse, nonspecific inflammatory disease of the mucosal lining of the colon and rectum
- most commonly involves the rectum, and may extend in a proximal and continuous fashion to involve
other parts of the colon
- Etiology
- unknown
- no bacterial or viral agent has been implicated
- family history is the most important risk factor
- altered immune response to external and host antigens may also play a role
- smoking is protective
- Pathology
- disease is confined to the mucosal and submucosal layers, sparing the muscularis
- begins in the rectum and may spread proximally to involve the entire colon
- terminal ileum is involved 10% of the time: ‘backwash ileitis’
- superficial ulcers and crypt abscesses are early pathologic signs
- Clinical Manifestations
- bloody diarrhea is the most common early symptom
- disease severity may range from mild disease with 4 or less bowel movements/day to severe disease with
10 or more stools/day with continuous bleeding
- other symptoms may include abdominal pain, weight loss, tenesmus, fever
- extraintestinal manifestations may also be present: arthritis, iritis, erythema nodosum,
pyoderma gangrenosum, hepatic dysfunction, sclerosing cholangitis
- usually presents as a chronic, low-grade illness in most patients; however, in 15% it may have an
acute and fulminating course
- Diagnosis
- stool studies are necessary to exclude infectious colitis
- colonoscopy is of value in determining the extent of disease but endoscopic biopsies will not usually
differentiate ulcerative colitis from Crohn’s colitis unless granulomas are seen
- rectal sparing and skip areas are most consistent with Crohn’s disease
- barium enema may show loss of haustral markings and ulcerations; in severe disease, the colon has the
appearance of a rigid tube (stovepipe colon)

- Medical Management
- acute attacks are usually treated with corticosteroids (40 to 60 mg prednisone QD)
- steroid enemas are effective in left colon disease or proctitis
- intravenous steroids are used in severe attacks for a period of 5 to 7 days
- sulfasalazine inhibits mucosal prostaglandin synthesis and is used to prevent relapses in
the chronic phase of disease
- immunomodulators such as azathioprine, 6-mercaptopurine, cyclosporine are used in steroid-unresponsive disease
- antitumor necrosis factor antibodies (infliximab) are used for maintenance therapy and as second line therapy in steroid-refractory UC
- antibiotics have no proven value in the treatment of ulcerative colitis
- Indications for Surgery
- removal of the entire colon and rectum cures ulcerative colitis
- Urgent or Emergent Indications
- Massive Hemorrhage
- rare, occurring in < 1% of patients
- 50% of patients also have toxic megacolon
- total abdominal colectomy with ileostomy is the usual procedure
- if bleeding from the rectum persists, emergency proctectomy may be required
- a completion proctectomy with pouch reconstruction can be done at a later date
- Toxic Megacolon
- Clinical Manifestations
- occurs in 6% to 13% of patients with ulcerative colitis
- symptoms include abdominal pain, severe diarrhea, distention
- signs include abdominal tenderness, fever, tachycardia, lethargy, and shock
- KUB usually shows dilatation of the transverse colon (>8cm)
- chronic steroid use can mask many of the signs and symptoms

- Management
- unless peritonitis is present, the initial therapy is medical
- fluid and electrolyte replacement, broad-spectrum antibiotics,
high-dose steroids, NG decompression, and serial abdominal films are the initial therapies
- if there is no improvement within 24 to 48 hours, then surgery is indicated
- total abdominal colectomy with an ileostomy and Hartmann’s pouch is associated with a lower mortality
rate than emergent total proctocolectomy
- the rectum should be divided as low as possible and a mushroom catheter left in place to help
prevent stump blowout
- Fulminating Acute Ulcerative Colitis
- an acute episode that is not responsive to IV steroids or biologic agents will require an emergent abdominal
colectomy, ileostomy, and Hartmann’s pouch
- Perforation
- may be associated with toxic megacolon
- abdominal colectomy with ileostomy
- Elective Indications
- Intractability
- most common indication for surgery
- chronic ulcerative colitis may become a physical and social burden to the patient
- persistent need for long-term medical therapy has many complications (and costs)
- continence-preserving surgical procedures are an option for many patients to consider
- extracolonic manifestations responsive to surgery include erythema nodosum, arthritis,
and eye disease
- primary sclerosing cholangitis and ankylosing spondylitis do not respond to surgery
- Carcinoma
- patients with ulcerative colitis have an increased risk of developing colon cancer,
which is frequently multifocal
- the likelihood of carcinoma developing is related to both the extent of colonic involvement
and the duration of the disease
- after 10 years of pancolonic disease, the risk of colon cancer is approximately 1% a year
- patients with chronic ulcerative colitis need routine surveillance colonoscopy with random 4 quadrant
mucosal biopsies every 10 cm
- the presence of dysplasia is an indication for proctocolectomy
- strictures are also frequently malignant, and are an indication for surgery
- Growth Retardation
- failure to mature and grow at an acceptable rate is an accepted indication for surgery in children
- Choice of Operation
- Subtotal Colectomy and Ileostomy
- operation of choice in emergency settings since it is the least morbid procedure
- another indication is in patients who have indeterminant colitis – this allows complete pathologic
examination of the colon to rule out Crohn’s disease
- may consider leaving a long rectal stump as a mucous fistula to avoid the risk of an intraperitoneal stump leak
- preserves the option for an ileal pouch-anal anastomosis (IPAA) after recovery
- Proctocolectomy and Ileostomy
- curative, since it removes all the diseased mucosa
- poorly accepted by patients and physicians
- a permanent ileostomy is difficult to manage
- significant complications of the procedure include injury to the pelvic parasympathetic nerves,
resulting in bladder and sexual dysfunction, and poor healing of the perineal wound
- to avoid pelvic nerve injury the mesorectum should be divided close to the rectal wall
and the dissection should avoid the pelvic side walls
- perineal wound problems may be reduced by performing an intersphincteric proctectomy
which preserves the levator ani and external sphincter muscles
- these muscles may then be used in the closure of the perineum
- procedure is limited to patients with significant comorbid disease, poor sphincter function, or concurrent rectal cancer
- Subtotal Colectomy with Ileorectal Anastomosis
- used as a compromise operation in patients who are not candidates for ileoanal anastomosis
(indeterminant colitis) and who refuse an ileostomy
- since pelvic surgery is associated with infertility secondary to adhesions, this approach may be chosen
by young women who want to have children – once her family is complete, then a completion proctectomy
and ileal pouch reconstruction can be performed
- advantages of this approach include avoidance of an ileostomy and normal sexual and bladder function
- however, there are many disadvantages to this procedure:
- proctitis is not eliminated and 25% of patients will require completion proctectomy
- risk of developing cancer remains in the rectal segment
- functional results vary, with some patients having intractable diarrhea
- Proctocolectomy and Continent Ileostomy
- goal is to avoid the need for an external appliance
- patients must manually evacuate the pouch
- associated with a high rate of technical complications requiring reoperation
- rarely performed today - most common indication is in patients who have had a failed ileoanal anastomosis
- Ileoanal Anastomosis (IPAA)
- operation consists of a near total proctocolectomy, endorectal ileal pouch-anal anastomosis,
and diverting loop ileostomy
- the advantages of this operation include elimination of almost all diseased mucosa, preservation of the
anorectal sphincter, and avoidance of a permanent ileostomy
- functional results are generally good: the average number of daily bowel movements is 5 and nocturnal
bowel movements is 1; daytime incontinence is rare, however, nocturnal seepage is much more common
- most frequent late complication is pouchitis, which can be cured in most cases by a short course
of metronidazole
- small bowel obstructions are frequent (20%)
- sexual dysfunction in males and infertility in females remain significant problems
- contraindicated in patients with Crohn’s colitis
- may be done open or laparoscopically
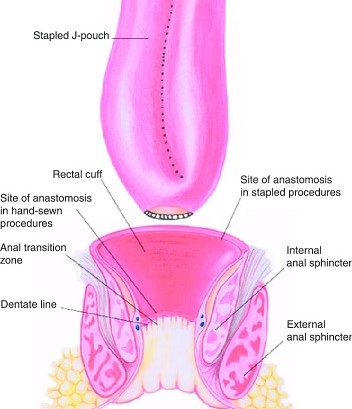
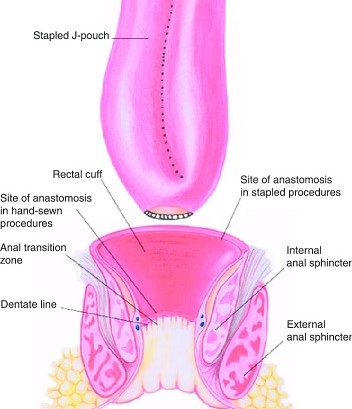
- J-Pouch Creation
- pouch is created with the last 30 cm of ileum using a GIA stapler
- imperative that the pouch reach the dentate line without tension
- posterior attachments of the small bowel mesentery must be mobilized up
to the third portion of the duodenum
- dividing the ileocolic artery near its origin with the SMA can give additional length
- relaxing incisions can also be made in the anterior and posterior surfaces of the mesentery
to gain additional length
- adequate length is confirmed when the apex of the pouch reaches past the symphysis pubis
- Ileal Pouch Anal-Anastomosis
- Double-Stapled anastomosis
- preserves the anal transition zone, which contains nerves for distinguishing between air, liquid, and stool
- associated with better postoperative continence, especially at night
- performed with the EEA stapler
- leaves behind a small amount of rectal mucosa that is at risk for development of dysplasia and cancer,
as well as inflammation
- known rectal dysplasia is a contraindication
- Mucosectomy and Hand-Sewn Anastomosis
- mucosa from the anal canal and distal rectum is excised transanally
- small islands of mucosa can be left behind, making scheduled pouchoscopy mandatory
- associated with higher rates of anastomotic stricture, septic complications, incontinence,
and pouch failure than a stapled anastomosis
- Ileostomy
- most surgeons use a protective ileostomy after IPAA
- ileostomy decreases the risk of pelvic sepsis from an anastomotic leak
- before ileostomy closure, the pouch must be assessed for healing – digital rectal exam, pouchoscopy,
contrast study
- some surgeons will skip the ileostomy in good risk patients
Crohn's Colitis
- Pathology
- 15% of patients with Crohn’s have disease limited to the colon
- characterized by transmural inflammation with aphthoid ulcers
- noncaseating granulomas are pathognomonic, as are fistulas
- discontinuous segmental involvement
- rectum is often spared (40%) and the ileum is often involved
- perianal disease is common
- 15% of cases cannot be differentiated from ulcerative colitis (indeterminate colitis)
- Clinical Manifestations
- abdominal pain, non-bloody diarrhea, and weight loss are the most common symptoms
- may present with complications of the disease: abscesses, fistulas, strictures
- toxic megacolon occurs less frequently than in ulcerative colitis
- Therapy
- neither medical therapy nor surgery is curative
- corticosteroids are the time-tested treatment for acute Crohn’s disease
- anti-TNF antibodies are used for inducing and maintaining remission in moderate to severe or
steroid-refractory disease
- surgery is limited to the treatment of complications and intractability
- Choice of Operation
- Proctocolectomy and Ileostomy
- procedure of choice for patients with intractable pancolonic disease or concomitant anorectal
and colonic disease
- also indicated if fecal incontinence is too severe to warrant preserving the rectum
- to reduce problems with nonhealing perineal wounds, an intersphincteric proctectomy may be performed
- an ileal pouch-anal anastomosis should not be done in a patient with Crohn’s disease because of the risk
of recurrence in the pouch and fistulas at the anastomosis
- likewise, a continent ileostomy should also not be done
- Segmental Resection
- segmental resection can be performed for patients with localized disease
- must accept the fact that recurrent disease in the colon is common
- 60% of patients require a second operation within 10 years
- good option for patients with limited disease who wish to avoid a stoma
- resection with diversion is appropriate for obstruction from a stricture
- Total Abdominal Colectomy with Ileorectal Anastomosis
- indicated in patients with rectal and anal sparing who wish to avoid an ileostomy
- patients must have good continence, because they will have multiple watery bowel movements
- will need frequent surveillance of the rectum for recurrence of CD, as well as for dysplasia and cancer
- ~50% of patients will require completion proctectomy and ileostomy within 10 years
References
- Sabiston, 20th ed., pgs 1339 - 1353
- Schwartz, 10th ed., pgs 1195 - 1201
- Cameron, 10th ed., pgs 154 - 160, 160 – 163, 163 – 168
- UpToDate. Surgical Management of Ulcerative Colitis. Phillip R. Fleisher, MD, FACS. Feb 24, 2020. Pgs 1 – 25