Management of Acute kidney Injury
Acute Kidney Injury (AKI)
- Definition
- an abrupt decline in the glomerular filtration rate
- usually defined as an increase in serum creatinine or a decrease in urine output
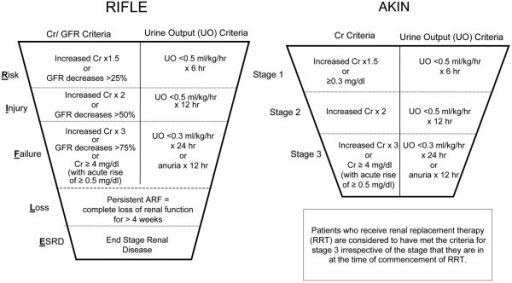
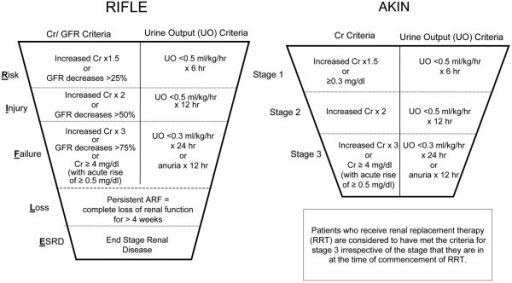
- several different staging systems exist (RIFLE, AKIN)
- Etiology
- Prerenal
- hypotension
- hypovolemia
- heart failure
- renal artery occlusion or stenosis
- Renal
- toxins (IV contrast dye, endotoxin)
- drugs (aminoglycosides, cyclosporine, amphotericin B, NSAIDs)
- pigment nephropathy (hemoglobin, myoglobin)
- Postrenal
- ureteral obstruction (stones, surgical injury)
- bladder dysfunction following pelvic surgery
- urethral obstruction (pelvic fractures, BPH)
- Diagnosis
- usually suspected in the postop setting by oliguria and/or a rising BUN/Cr
- evaluation begins with a review of the clinical course and a detailed exam of input/output and
medication records
- physical examination focuses on volume status and cardiac performance
- Laboratory Studies
- Urinalysis
- useful in selected cases
- detects free hemoglobin or myoglobin
- presence of casts denotes tubular necrosis
- sodium, creatinine, urea, and osmolality should be measured on each sample
- Urine Osmolality
- patients with prerenal AKI are more likely to have a concentrated urine > 500 mOsm/L
- not very discriminating - there is a lot of overlap between patients with prenal and renal AKI
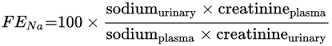
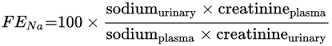
- Fractional Excretion of Sodium (FeNa)
- under normal circumstances the fractional excretion of sodium is less than one percent of
the filtered load
- FeNa > 3 suggests a renal or postrenal etiology
- FeNa < 1 suggests a prerenal etiology
- Radiology
- Ultrasound
- useful for evaluating for obstruction by detecting hydronephrosis
- Doppler may be used to evaluate renal blood flow in kidney transplant patients and trauma patients
- Additional Studies
- radionuclide scans and arteriography may be useful in selected patients
- Prevention Strategies
- Prevention of Contrast-induced Nephropathy
- high osmolar agents should be avoided
- volume expansion with an isotonic fluid is the primary preventive strategy
- N-acetylcysteine, a free-radical scavenger, is often used in addition to volume expansion,
but it is of unproven benefit
- Additional Preventive Strategies
- Fluid Resuscitation
- most important priority is to maintain renal perfusion
- early and aggressive fluid resuscitation in trauma and sepsis is associated with a
lower incidence of AKI
- Diuretics
- mannitol has documented efficacy in preventing AKI in renal transplant patients and
patients with rhabdomyolysis
- diuretics are contraindicated in hypovolemic patients
- Fenoldopam
- increases renal blood flow by stimulating dopamine receptors in the kidney
- may reduce AKI after cardiac surgery and liver transplantation, but does not appear to
reduce mortality or the need for dialysis
- Indications for Dialysis
- Indications
- volume overload unresponsive to diuretics
- life-threatening hyperkalemia
- severe acidosis (pH < 7.1)
- uremic encephalopathy or pericarditis
- ± BUN > 100 mg/dl
- Types of Dialysis
- no one form of dialysis has been proven superior to another in patients with AKI
- Hemodialysis (HD)
- very efficient at removing volume, electrolytes, and toxins
- method of choice in the hypercatabolic patient
- requires a double-lumen venous dialysis catheter
- complications include hypotension, bleeding, dysequilibrium syndrome due to osmolarity
changes, and arrhythmias
- Peritoneal dialysis (PD)
- much less efficient than hemodialysis, but is well-tolerated hemodynamically
- however, PD is a 12- to 24-hour continuous therapy, which mitigates its inherent inefficiencies
- rarely used in critically ill surgical patients because it requires an intact peritoneal
cavity
- Continuous Renal Replacement Therapy (CRRT)
- avoids much of the hemodynamic instability of HD
- other potential advantages include more consistent salt and water removal, and enhanced
clearance of inflammatory mediators
- no documented survival advantage to CRRT over HD
- Continuous Venovenous Hemofiltration
- positive hydrostatic pressure drives water and solutes across the filter membrane
- the flow of water across the membrane drags solutes along (convection)
- advantages include smooth, continuous fluid removal with minimal hypotension
- requires a large central venous dialysis catheter and a blood pump to drive blood
flow through the filter
- Continuous Venovenous Hemodiafiltration
- adds a dialysate flow to supplement hemofiltration
References
- Simmons and Steed, pgs 270 - 284
- Cameron, 13th ed. pgs 1404 - 1409
- UpToDate. Overview of the Management of Acute Kidney Injury in Adults. Okusa, Mark and
Rosner, Mitchell. Nov 16, 2017. Pgs 1 – 22.
- UpToDate. Renal Replacement Therapy (Dialysis) in Acute Kidney Injury in Adults: Indications, Timing,
and Dialysis Dose. Palavesky, Paul. Nov 05, 2018. Pgs 1 – 23.