Pulmonary Physiology, Ventilators, ARDS
Anatomy
- Pulmonary Circulation
- the lung has a dual circulation, bronchial and pulmonary
- Bronchial Circulation
- bronchial arteries arise from the aorta or upper intercostal arteries
- supplies the airways up to the terminal bronchioles
- most of the bronchial venous return is via bronchial veins into the azygous, hemiazygos, or
intercostal veins
- a small fraction of this venous blood drains directly into the pulmonary veins, creating a
physiologic shunt
- the lung can tolerate the loss of its bronchial blood supply without significant dysfunction
- Pulmonary Circulation
- lungs receive the entire cardiac output from the right ventricle
- high flow, low pressure circuit (mean PA pressure = 15 mm Hg)
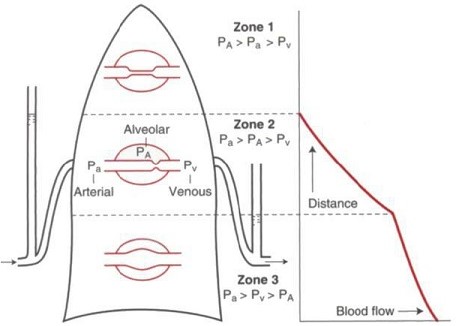
- gravitational forces play an important role in the distribution of pulmonary blood flow
- there is a gradient of increasing hydrostatic pressure from the apex of the lung to its base
in the upright patient
- this creates several zones based on the dynamic between alveolar distending pressure,
pulmonary artery pressure, and pulmonary venous pressure:
- Zone 1
- occurs at the apex of the lung
- blood flow in the apex is minimal because of low perfusion pressures
- blood flow can be reduced to zero if alveolar pressure rises above pulmonary artery
pressure (PA > Pa > Pv)
- this does not normally occur
- however, if arterial pressure is reduced (hypovolemia) or alveolar pressure is
raised (mechanical ventilation), then zone 1 conditions can occur
- zone 1 regions function as dead space: areas of ventilated but not perfused lung
- Zone 2
- pulmonary artery pressure increases due to the hydrostatic gradient and is greater
than alveolar pressure
- venous pressure remains below both the arterial and alveolar pressures
(Pa > PA > Pv)
- blood flow is determined by the difference between the pulmonary artery and alveolar
pressure
- Zone 3
- pulmonary artery and venous pressures are both greater than alveolar pressure
(Pa > Pv > PA)
- alveolar pressure has no role in determining blood flow in zone 3
Pulmonary Mechanics
- Lung Volumes
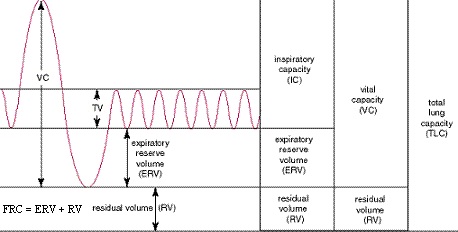
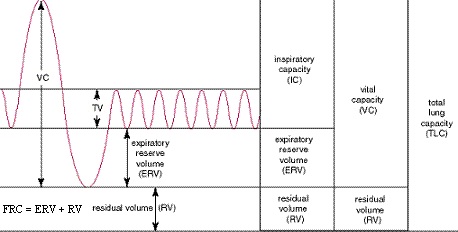
- total lung capacity (TLC) = the volume of gas contained within the lung at maximal inspiration
- vital capacity (VC) = greatest volume that can be exhaled during a maximal respiratory effort
- residual volume (RV) = amount of gas remaining in the lung after a maximal exhalation
- functional residual capacity (FRC) = amount of gas remaining in the lung after a normal exhalation –
represents the point in the respiratory cycle when the lung elastic recoil and chest outward expansion are equal
- expiratory reserve volume (ERV) = amount of gas that can be exhaled after a normal breath
- tidal volume (TV) = amount of air moved during a normal breath
- inspiratory reserve volume (IRV) = amount of air that can be inhaled after a normal inhalation
- inspiratory capacity (IC) = amount of air that can be inhaled after a normal breath
- Functional Residual Capacity
- residual alveolar air allows the alveoli to remain open
- if FRC falls below airway closing capacity, then alveoli collapse and airway resistance increases
- decreased FRC results in atelectasis and shunts
- conditions that predispose to decreased FRC include supine positioning, increased abdominal pressure
(ascites, compartment syndrome, obesity), and decreased chest wall elastic recoil (surgical incisions,
burns, kyphoscoliosis)
- Mechanical Properties of the Lung and Chest Wall
- Lung
- elastic structure with an inherent tendency to recoil any time that it is stretched beyond
its resting volume
- inward recoil is due to elastic fibers within the lung and surface tension forces within the
alveoli
- surface tension forces are created by the air interface with the liquid film lining the
alveoli
- surfactant lowers these surface tension forces, making it easier to inflate the lung
- Chest Wall
- also an elastic structure that has a tendency to return to its resting position when
displaced from it
- resting position of the chest wall occurs at ~ 75% of the vital capacity
- at lower volumes, there is a tendency for the chest wall to recoil outward; at higher volumes
the chest wall recoils inwards towards its resting volume
- Total System
- elastic properties of the total respiratory system are defined by the interplay between the
lungs and chest wall
- at most lung volumes the thorax has an outward recoil force and the lungs have an inward
recoil force
- balance between these 2 opposing forces results in a slightly negative resting intrathoracic
pressure
- FRC is achieved when the inward tendency of the lung to recoil is exactly balanced by the
outward tendency of the chest wall to expand
- it is not until over 75% of the vital capacity is obtained that both the lung and chest wall
recoil in the same direction
- deformities of the chest wall (kyphoscoliosis, obesity) can have important effects on lung
volumes
- restrictive lung diseases (pulmonary fibrosis) increase the elastic recoil of the lung and
thus decrease FRC
- emphysema decreases the elastic recoil of the lung and thus increases FRC
Ventilation
- Control
- normal ventilation is involuntary and is mediated by the dorsal nucleus and ventral nucleus in the
medulla
- peripheral chemoreceptors in the carotid bodies are solely responsible for the hypoxic ventilatory
response
- central chemoreceptors in the medulla increase ventilation in response to increased arterial
CO2 or decreased pH
- Inspiration
- initiated with contraction of the inspiratory muscles (diaphragm, external intercostals)
- expansion of the chest increases the negative intrathoracic pressure, creating a pressure gradient
down which fresh air flows into the lung
- inspiration ceases when alveolar pressure equals atmospheric pressure
- basilar alveoli are better ventilated than apical alveoli
- stretch receptors within the lung also produce feedback signals to shut off inspiration
(Hering-Breuer reflex)
- resistance to flow occurs in the nose, upper airway, and larger parenchymal airways
- bronchial smooth muscle tone affects airway diameter and therefore airway resistance
- Expiration
- purely passive
- relaxation of the inspiratory muscles and elastic recoil of the chest produces a positive alveolar
pressure that forces air out of the airways
- expiration ceases when the inward recoil pressure of the lung equals the outward recoil forces of
the chest wall
- during maximal exhalation, flow is effort dependent until dynamic compression of the airways occurs
- Minute Ventilation
- total amount of air moved per minute (Ve = TV x RR)
- combination of the volume of air in the dead space and functional alveoli
- arterial PCO2 levels are inversely proportional to the effectiveness of alveolar ventilation
- for a given minute ventilation, the higher the respiratory rate, the less effective the alveolar
ventilation (most of the respiratory effort is spent moving air through the physiologic dead spaces)
Respiration (Gas Exchange)
- Diffusion
- large surface area of the lung, as well as its thin surface, make it uniquely constructed for rapid
diffusion
- average erythrocyte traverses the pulmonary capillary in 0.75 seconds
- diffusion equilibrium for oxygen occurs within 0.25 seconds
- lung has a large reserve before diffusion becomes limited
- most processes that limit diffusion involve loss of functional membrane area (i.e. surgical resection)
- pathologic thickening of the diffusing membrane is rarely the cause of hypoxemia
- Ventilation/Perfusion Mismatches
- major cause of abnormal gas exchange in clinical medicine
- in the perfect lung, the level of perfusion would exactly match the level of ventilation so that
maximal transfer of oxygen and carbon dioxide could occur
- all lungs have some mismatching of ventilation and perfusion, resulting in some inefficiency of gas
exchange
- in the normal lung, both blood flow and ventilation are increased at the base and decreased towards
the apex
- the rate at which ventilation and perfusion change as one moves from base to apex is not uniform
- blood flow falls off more rapidly, resulting in an increasing ratio of ventilation to perfusion
(V/Q) from the base to the apex
- Dead Space
- regions of the lung that are overventilated (high V/Q) relative to their perfusion
- anatomic dead space is composed of all the airways without alveoli
- alveolar dead space is composed of alveoli that are ventilated but not perfused
- physiologic dead space is the sum of the anatomic and alveolar dead space
- ventilation of dead space decreases the amount of ventilation available to better perfused
areas of the lung, in effect lowering alveolar ventilation
- normal ratio of dead space to tidal volume is 0.2 to 0.35
- processes that can increase dead space include endotracheal tubes, pulmonary embolism,
hypoperfusion, and diseases that destroy the pulmonary vasculature
- Shunts
- regions where perfusion greatly exceeds ventilation (V/Q < 1)
- a portion of the perfusion is ‘wasted’ as it is not adequately exposed to alveolar gas for
full equilibration to occur
- shunts may be described as anatomic or physiologic
- anatomic shunts are those where desaturated blood is directly mixed with oxygenated blood
through direct vascular connections (patent foramen ovale)
- there are two normal anatomic shunts: 1) bronchial venous return enters the pulmonary veins
without going through the lungs, 2) coronary veins (thebian veins) empty directly into the
left atrium)
- physiologic shunts (venous admixture) are those where desaturated blood returns to the
pulmonary venous system without having been oxygenated
- the effect of a physiologic shunt is to return unoxygenated blood to the left atrium
- some causes of an increased shunt fraction include atelectasis (alveolar collapse),
pneumonia, alveolar edema)
- in a pure shunt (V/Q = 0), administration of 100% oxygen will not improve the situation
Acute Respiratory Failure
- Hypoxemic Respiratory Failure (Type I)
- most common type of respiratory failure
- defined as PaO2 < 60 mm Hg on room air
- etiologies include pneumonia, atelectasis, aspiration, pulmonary edema
- treatment goal is an arterial oxygen saturation > 90% on the lowest FIO2 possible
- Hypercapnic Respiratory Failure (type II)
- defined as a PaCO2 > 50 mm Hg on room air
- etiologies include over sedation, COPD, mental status changes
- many of these patients are hypoxemic as well
- treatment goal is to increase alveolar ventilation by increasing minute ventilation
Management of Acute Respiratory Failure
- Noninvasive Ventilation
- provides positive pressure ventilation without the need for an invasive airway
- should be considered a bridging therapy
- if the underlying cause of hypoxemia or ventilatory failure cannot be treated quickly, then a
definitive airway will be necessary
- Continuous Positive Airway Pressure (CPAP)
- provides a continuous level of positive pressure through a tight-fitting mask
- maintains a patient’s functional residual capacity (FRC)
- improves oxygenation, but not ventilation
- useful adjunct for treating pulmonary edema while being diuresed
- BiPAP
- maintains FRC
- also adds a driving pressure when the patient initiates a breath, which can improve
ventilation
- effective in treating hypercapnic respiratory failure
- first-line of therapy for COPD exacerbations
- Mechanical Ventilation
- Methods to Improve Oxygenation
- ↑ FIO2
- goal is arterial saturation > 90% on the lowest FIO2 possible
- FIO2 levels > 50% are associated with oxygen toxicity and absorption
atelectasis
- ↑ PEEP
- increases mean airway pressure, which prevents small airway collapse and maintains or
increases FRC
- high PEEP levels can result in barotrauma
- ↑ I:E Ratio
- increases inspiratory time
- normal I:E ratio is 1:2
- increases oxygenation
- may lead to increased ventilator-induced lung injury (VILI) by increasing lung
stress
- Methods to Improve Ventilation
- increase minute ventilation by increasing tidal volume or respiratory rate
- eliminate dead space
- at high respiratory rates, the lungs can become hyperinflated because of decreased time
for expiration
- Modes of Ventilation
- air is delivered under positive pressure against the compliance of the lung
- positive pressure ventilation can be delivered via a volume or pressure target
- Volume Modes
- tidal volume is set and guaranteed, while airway pressure is variable
- barotrauma can result from high peak airway pressures
- Assist Control Ventilation (AC)
- delivered tidal volume is the same whether patient triggered or time triggered
- ventilator delivers breaths in coordination with the respiratory effort of the
patient
- a patient with a high respiratory rate can hyperventilate and develop a severe
respiratory alkalosis
- may generate high levels of autopeep (caused by incomplete exhalation at rapid
respiratory rates)
- if the patient does not trigger a breath within the set time interval, then the
ventilator will deliver a breath
- Synchronous Intermittent Mandatory Ventilation (SIMV)
- intersperses spontaneous breaths with machine breaths
- SIMV synchronizes the breaths to avoid stacking a ventilator breath on top of a
spontaneous breath
- pressure support can be added to spontaneous breaths
- felt to maintain respiratory muscle activity and prevent atrophy
- provides a well-tolerated method for weaning from the ventilator
- Pressure Modes
- airway pressure is set and tidal volume is variable
- changes in airway pressure can cause rapid changes in tidal volume and minute ventilation,
resulting in acute respiratory acidosis
- Pressure Control Ventilation
- avoids high peak and plateau airway pressures and subsequent barotrauma
- delivered tidal volume is dependent on lung compliance
- standard inspiration to expiration ratio usually is reversed from 1:2 to greater
than 1:1
- prolonging inspiration promotes gas distribution and shortening expiration lessens
alveolar collapse (autopeep)
- associated with decreased minute ventilation because of decreased tidal volumes
and a concomitant rise in PCO2
- Pressure Support Ventilation
- breaths are assisted by a set inspiratory pressure
- respiratory rate and tidal volume are determined by the patient
- can be used as a stand-alone mode, or in conjunction with SIMV
- limits barotrauma and decreases the work of breathing
- apnea alarm must be set because the ventilator does not deliver a timed breath
- used at low levels in spontaneous breathing trials
- Positive End Expiratory Pressure (PEEP)
- valve maintains positive pressure in the airways at all times, including at the end of expiration
- positive alveolar pressure at the end of expiration prevents alveolar collapse, recruits FRC, and
decreases the intrapulmonary shunt fraction
- PEEP may allow the reduction of FIO2 to nontoxic levels
- a negative side effect of PEEP is decreased venous return to the heart and a lowered cardiac output
- PEEP is also associated with barotrauma
Acute Respiratory Distress Syndrome (ARDS)
- Criteria for Diagnosis
- acute, bilateral pulmonary infiltrates on CXR or CT scan
- absence of CHF or volume overload
- mild ARDS: PaO2/FIO2 ratio = 201 – 300 mm Hg; PEEP ≥ 5 cm H2O
- moderate ARDS: PaO2/FIO2 ratio = 101 – 200 mm Hg; PEEP ≥ 5 cm H2O
- severe ARDS: PaO2/FIO2 ratio ≤ 100 mm Hg; PEEP ≥ 5 cm H2O

- Pathogenesis
- coincides with acute onset of respiratory failure
- disruption of the alveolar epithelium results in influx of protein-rich fluid and leukocytes into
the alveolus
- destruction of type 2 pneumocytes disrupts surfactant production, contributing to alveolar flooding
and collapse
- alveolar macrophages release proinflammatory cytokines that attract and activate neutrophils,
provoking tissue injury and the formation of hyaline membranes
- Management
- Low Tidal Volume Ventilation
- high tidal volumes can lead to VILI from overstretching alveoli (volutrauma)
- multicenter ARMA trial documented lower mortality if a tidal volume of 6 mL/kg is used,
instead of the more traditional 12 mL/kg
- respiratory rate must be increased to maintain minute ventilation
- peak plateau pressures should be kept ≤ 30 cm H2O
- FIO2 and PEEP are adjusted to keep the O2 sats > 88%
- Permissive Hypercapnia
- low tidal volumes can result in decreased minute ventilation, leading to hypercapnia and
respiratory acidosis
- hypercapnia is tolerated in order to reduce alveolar overdistention and volutrauma
- respiratory acidosis is treated by increasing minute ventilation or adding bicarbonate
infusion
- since hypercapnia can increase intracranial pressure, it must be avoided in patients with a
head injury
- PEEP
- improves oxygenation by recruiting collapsed alveoli, increasing FRC, and reducing
ventilation-perfusion mismatches
- complications of high levels of PEEP include barotrauma, alveolar overdistention, and
decreased cardiac output
- in ARDS, higher levels of PEEP may have beneficial effects on outcome
- Management of Refractory Hypoxemia
- Salvage Modes of Ventilation
- airway pressure release ventilation (APRV) and high-frequency oscillatory ventilation (HFOV)
have been used when other modes of mechanical ventilation fail
- both use higher mean airway pressures and small tidal volumes with the goal of reducing
volutrauma
- no convincing evidence that these rescue modes improve mortality
- Recruitment maneuvers
- brief application of a high level of continuous positive pressure airway pressure in order
to open up collapsed alveoli
- a common method is to provide 30 – 40 cm H2O PEEP for 30 – 40 seconds
- oxygenation generally improves after a recruitment maneuver, but there is no evidence of
improved mortality
- Prone Positioning
- may improve oxygenation by redistributing perfusion to ventilated lung, thereby reducing
intrapulmonary shunting
- recent studies have shown a decreased mortality rate
- labor intensive
- tube dislodgement during positioning is a major concern
- positioning difficulties also arise in patients with open abdomens or unstable spine injuries
- Inhaled Nitric Oxide
- pulmonary vasodilator
- decreases pulmonary vascular resistance, pulmonary artery pressure, and right ventricular
afterload
- may improve oxygenation without affecting mortality
- Extracorporeal Membrane Oxygenation (ECMO)
- considered when all other rescue strategies have failed
- provides oxygenation and ventilation while the lung recovers
- since patients must be anticoagulated, bleeding complications are common
(intracranial hemorrhage)
Ventilator-Associated Pneumonia (VAP)
- Definition
- pneumonia that develops 48 hours after intubation
- incidence is 1% - 3% per ventilator day
- mortality rate may be as high as 50%
- Diagnosis
- surprisingly difficult diagnosis to make in the ICU
- new onset hypoxia, purulent sputum, fever, ↑ WBC, and CXR infiltrates will strongly suggest VAP
- however, acute lung injury, CHF, PE, and tracheobronchitis may share similar findings
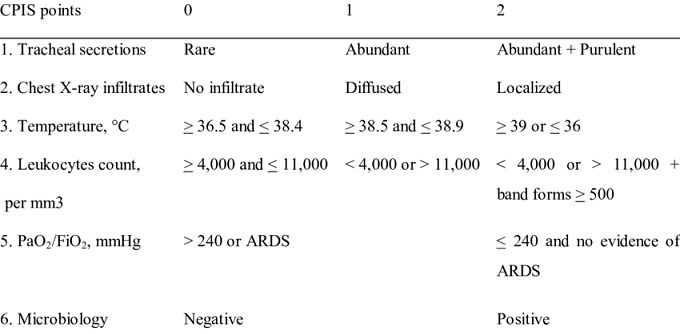
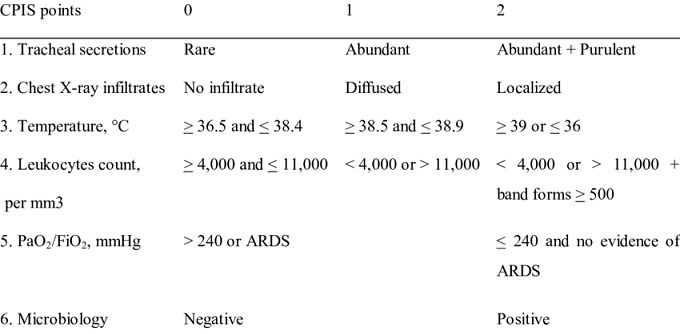
- Clinical Pulmonary Infection Score (CPIS)
- CPIS score ≥ 6 is highly predictive of VAP
- Culture Collection
- fiberoptic bronchoscopy with bronchoalveolar lavage (BAL) has long been the gold standard
for obtaining cultures
- blind bronchial brushings and blind endotracheal aspirates appear to be as accurate as the
more invasive BAL
- Antibiotic Management
- empiric antibiotics should be started as soon as VAP is suspected
- therapy should be deescalated once a specific microorganism is identified
- a 7 or 8 day course of antibiotics will be sufficient for most patients
- Choice of Antibiotics
- S. aureus is the most common pathogen isolated (25%), and should be covered with vancomycin
or Linezolid
- P. aeruginosa should be double covered
- Prevention
- Basic Measures
- avoid intubation by using CPAP or BiPAP when feasible
- minimizing sedation
- spontaneous breathing trials with no sedation
- head of bed elevation to 30 – 45 degrees
- minimizing pooling of secretions above the endotracheal tube
- changing the ventilator circuit only if dirty or malfunctioning
- Special Approaches
- evidence is less clear that the following interventions improve outcomes:
- oral care with chlorhexidine
- selective decontamination of the digestive tract
- ETT cuff pressure between 20 – 30 cm H2O
- silver-coated endotracheal tubes
References
- O’Leary, pgs 376 – 405
- Simmons and Steed, pgs 163 - 177
- Mattox, 4th ed., pgs 1321 – 1327
- Cameron, 13th ed., pgs 1379 - 1388
- UpToDate. Mechanical Ventilation of Adults in Acute Respiratory Distress Syndrome. Siegel, Mark
and Hyzy, Robert. Nov. 08, 2017. Pgs 1 – 41.
- UpToDate. Risk Factors and Prevention of Hospital-Acquired and Ventilator-Associated Pneumonia in
Adults. Klompas, Michael. March 07, 2019. Pgs 1 – 24.