Pathophysiology of Shock
- Definition of Shock
- circulation fails to deliver to cellular mitochondria sufficient oxygen to sustain aerobic
metabolism
- many different etiologies exist, but the ultimate result is a dysfunction of cellular biochemistry
leading to acidosis and decreased energy (ATP) production
- Aerobic and Anaerobic Metabolism
- Aerobic Metabolism
- for energy, cells depend on the hydrolysis of high energy phosphate bonds from ATP
- the hydrolysis of ATP also results in the production of a proton
- in normal circumstances, oxidative phosphorylation (aerobic metabolism) reclaims the proton
in resynthesis of ATP from ADP
- oxidative phosphorylation is dependent on oxygen, since oxygen is the final electron
acceptor in the electron transport chain
- glycolysis converts glucose to 2 pyruvates, producing a net gain of 2 ATP
- when cellular oxygen delivery is sufficient, pyruvate crosses the mitochondrial membrane and
enters the energy efficient Krebs cycle
- net result is production of 38 ATP from 1 glucose molecule
- Anaerobic Metabolism
- if there is insufficient cellular oxygen to support aerobic metabolism, pyruvate cannot
enter the Krebs cycle
- anaerobic glycolysis is inefficient, only producing 2 ATP from each glucose molecule
- Acidosis
- ATP hydrolysis is the source of acidosis in cellular hypoxia
- inefficient regeneration of ATP allows the accumulation of H+ in the cell
- pyruvate is converted to lactate, which buffers the excess protons and is
converted to lactic acid
- production of lactate is not the cause of cellular acidosis, but rather is a marker
of the magnitude of shock
- acidosis will affect calcium signaling and normal hormone and enzyme functioning
- Consequences of Decreased ATP Production
- all ATP-dependent cell processes are affected, including maintenance of the cell
membrane potential, cell signaling, synthesis of proteins and enzymes, and
DNA repair mechanisms
- gene transcription will also be affected
Sepsis and Septic Shock
- Definitions
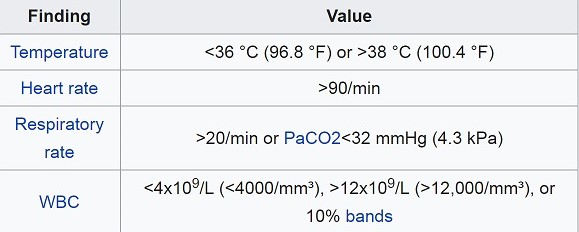
- Systemic Inflammatory Response Syndrome (SIRS)
- clinical syndrome that is a form of dysregulated inflammation
- no longer considered the earliest form of sepsis since it may be present in noninfectious conditions as
well (pancreatitis, surgery, trauma, burns)
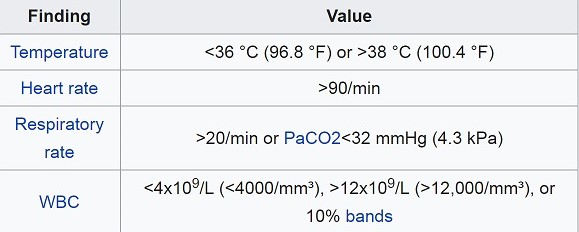
- defined as two or more abnormalities in temperature, heart rate, respiratory rate, and WBC count:
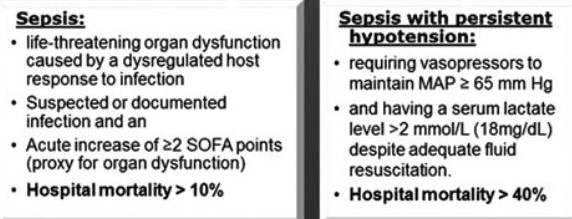
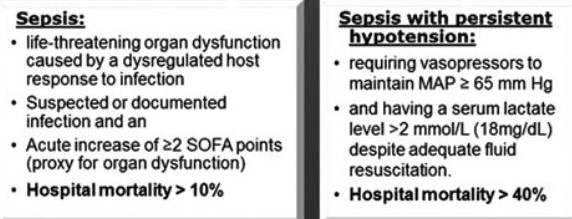
- Sepsis
- defined as a life-threatening organ dysfunction caused by a dysregulated host
response to infection
- continuum of severity ranging from infection, bacteremia, sepsis, and septic shock
- these new definitions are controversial, and have not yet been endorsed by many important
societies
- Pathophysiology
- the inflammatory response to infection or tissue injury is mediated by cells of the innate immune
system: macrophages, monocytes, and neutrophils
- these cells elaborate numerous inflammatory and anti-inflammatory cytokines
- when the local proinflammatory response exceeds the ability of the local anti-inflammatory response
to contain the inflammatory process, the inflammatory response becomes systemic
- the systemic release of proinflammatory cytokines leads to the alterations seen in sepsis and septic
shock: fever, leukocytosis, increased cardiac output, decreased peripheral vascular resistance,
tachycardia, hyperglycemia, and organ dysfunction
- Risk Factors
- ICU admission
- bacteremia
- age ≥ 65
- immunosuppression
- diabetes
- obesity
- malignancy
- previous hospitalization within 90 days
- Diagnosis
- often made empirically at bedside using a constellation of clinical, laboratory, radiologic,
physiologic, and microbiologic data
- the identification of a culprit organism occurs in less than 50% of cases
- Clinical Presentation
- typical presentation includes tachycardia, fever, and hypotension
- in the early stages of sepsis, the skin may be warm
- signs of organ dysfunction may also be present: oliguria, respiratory insufficiency,
altered mentation
- Laboratory Evaluation
- there is no single laboratory test that is diagnostic of sepsis
- CBC with differential, electrolytes, liver function tests, and coagulation studies may
support the diagnosis and indicate the severity of organ dysfunction present
- ABGs will indicate the degree of acidosis, hypoxemia and hypocarbia present
- lactate may also indicate the degree of sepsis and is useful for following the therapeutic
response
- blood cultures should be obtained from peripheral sites as well as from any
central lines
- urine, sputum, and wound cultures should be obtained as clinically indicated
- Imaging
- CXR to evaluate for pneumonia
- CT scan to look for drainable fluid collections in the abdomen or chest
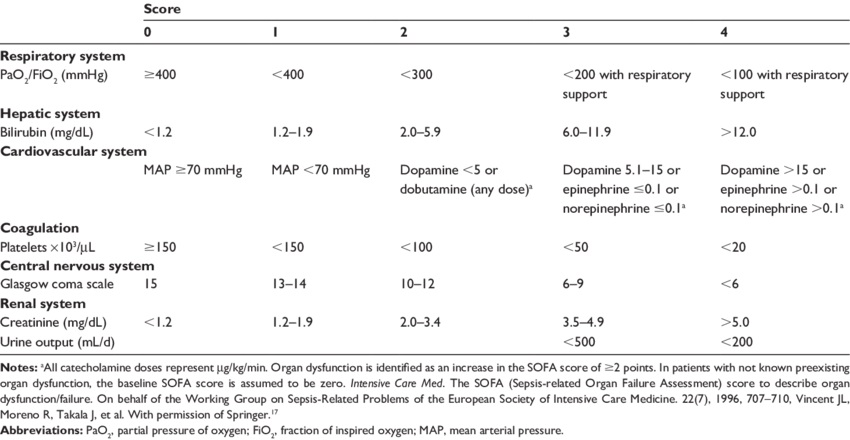
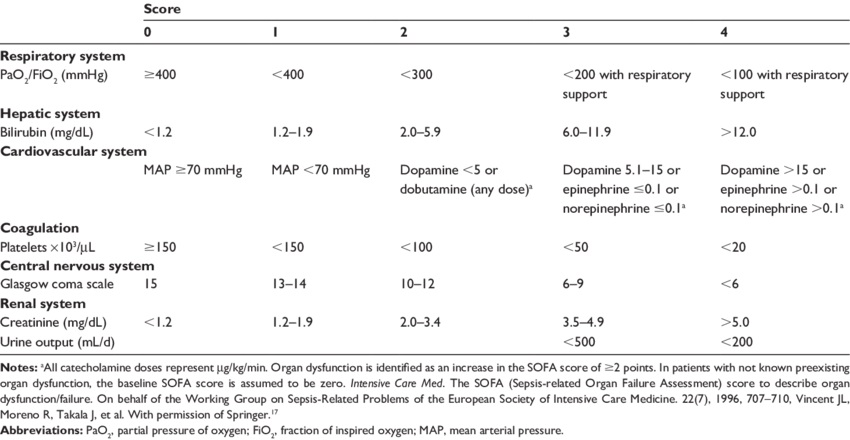
- Sequential Organ Failure Assessment (SOFA) Score
- used more in critical care research than at the bedside
- sepsis-3 definition of sepsis requires an acute increase of 2 or more SOFA points, which is
a marker for organ dysfunction
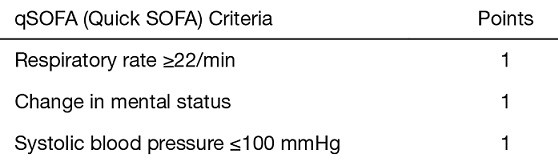
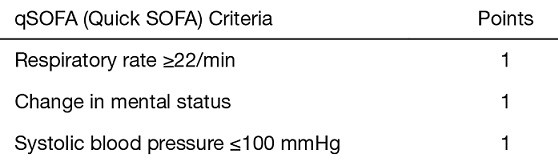
- Quick SOFA (qSOFA) Score
- developed as a simple screening tool to identify patients with possible sepsis
- qSOFA score ≥ 2 identifies patients at high risk for a poor outcome
- importantly, the qSOFA score has failed validation in several large studies
- Management
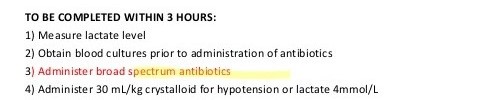
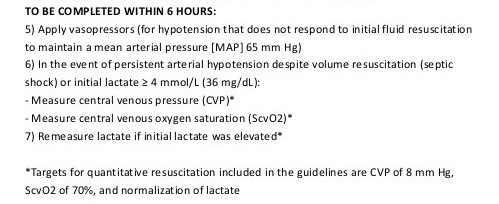
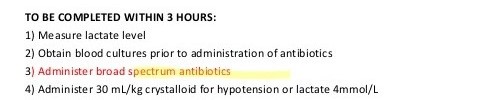
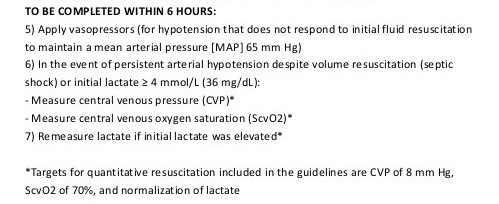
- Surviving Sepsis Campaign Bundles
- outlines tasks to be completed within 3 and 6 hours
- early identification of patients with sepsis, early IV fluid administration, early IV antibiotic
administration, and early source control are the goals of sepsis management
- ABCs
- secure the airway, if necessary
- administer supplemental oxygen and monitor with continuous pulse oximetry
- patients who require mechanical ventilation should be managed like ARDS patients (low tidal
volumes (6 mL/kg) and low peak plateau pressures (< 30 cm H2O))
- most patients will require a central line for fluids, pressors, and blood products
- the central line can also be used for CVP and central venous oxyhemoglobin saturation
(ScvO2) monitoring
- Fluid Resuscitation
- after securing the airway, restoration of circulatory volume is the next priority
- 30 mL/kg of crystalloid should be infused over 3 hours for hypotension or a
lactate ≥ 4 mmol/L
- additional fluid boluses should be given as necessary
- blood transfusions should be limited to patients with a Hg < 7
- initial resuscitation endpoints are a MAP ≥ 65 mm Hg or a urine output of 0.5 mL/kg/hr
- a normal serum lactate also indicates adequate resuscitation
- if a central line is in place, a CVP of 8 – 12 and a ScvO2 of 70% also indicate adequate
resuscitation
- Antibiotics
- empiric antibiotics are given based on the most likely pathogens
- antibiotics should be given within 1 - 3 hours of presentation
- empiric antifungal therapy is indicated in immunocompromised patients
- coverage should be narrowed once culture data is available
- Vasopressors
- will be necessary if hypotension does not respond to fluids
- norepinephrine is usually the first choice
- septic patients may be resistant to catecholamines
- vasopressin is added in norepinephrine-resistant patients
- occasionally the addition of an inotrope like dobutamine or milrinone can increase tissue
perfusion
- Source Control
- IV antibiotics are not usually sufficient treatment in surgical patients
- abscesses must be drained, infected catheters removed, and dead tissue debrided as soon as possible
- Glucose Control
- insulin resistance and hyperglycemia are typical in critically ill and septic patients
- goal of treatment is a glucose between 140 – 180 mg/dL, which prevents most episodes of
hypoglycemia
- Corticosteroids
- sepsis is often associated with adrenal insufficiency
- multiple studies have shown conflicting results about the efficacy of steroids in patients
with sepsis
- hydrocortisone 200 mg in divided doses can be considered in patients with hypotension refractory
to fluids and pressors
- Immune Modulation
- antiendotoxin antibodies, anticytokine antibodies, cytokine receptor antagonists,
nitric oxide synthase inhibitor, O2 radical scavengers have all been developed to treat
sepsis
- to date, these agents have not shown efficacy in human trials
Multiple Organ Dysfunction Syndrome (MODS)
- Pathophysiology
- most common cause of death in SICUs
- appears to be the final pathway to death after sepsis, SIRS, and trauma
- studies have identified microvascular thrombosis and end organ ischemia as the histopathological
features of MODS
- the actual mechanism of MODS remains unclear
- one current theory proposes that cellular hypoxia leads to mitochondrial injury, which in turn
results in dysfunction in oxidative metabolism
- Clinical Features
- there is a spectrum of organ dysfunction, from mild and reversible to complete failure
- the organ systems most commonly involved are the lungs, liver, kidneys, cardiovascular system, CNS,
and bone marrow
- organ dysfunction typically begins 24 – 48 hours after the origin of the insult
- most commonly, the lungs are the first organ affected, followed by the liver and kidneys
- Organ System Dysfunction
- Acute Lung Injury
- Definition
- characterized by hypoxemia
- stratified by the ratio of partial pressure of oxygen to the fraction of inspired
oxygen (PaO2/FiO2)
- ARDS = PaO2/FiO2 < 100
- Management
- goal is to maintain the oxygen saturation > 92%
- a second goal is to minimize barotrauma and oxygen toxicity
- ventilator management includes the use of PEEP, low tidal volumes, and airway
pressures < 30 cm H2O
- Acute Kidney Injury
- Definition
- stratified by the serum creatinine level and urine output
- creatinine ≥ 5 or a urine output < 200 ml/d represents the highest degree
of renal injury, and carries a high mortality rate
- Management
- maintain renal perfusion to avoid worsening the injury
- avoid nephrotoxic drugs
- continuous renal replacement therapy is often used in unstable patients, but it has
not been shown to be superior to intermittent hemodialysis
- Liver Dysfunction
- Definition
- stratified by the serum bilirubin concentration
- total bilirubin > 12 corresponds to the highest degree of liver injury
- etiology is likely related to splanchnic vasoconstriction and hypoperfusion
- ‘shock’ liver initially presents with elevated transaminases, followed by increasing
bilirubin
- synthetic dysfunction (↑ INR) is a later finding
- Management
- supportive care involves maintaing perfusion, avoiding hepatotoxins, providing
nutrition, and managing encephalopathy
- Cardiovascular Dysfunction
- Definition
- characterized by the MAP and the need for pressors
- Management
- initial management is with the use of fluids to support blood pressure
- norepinephrine is the preferred pressor agent
- vasopressin is added when norepinephrine alone cannot keep the MAP > 65
- invasive monitoring with pulmonary artery catheters has not improved outcomes
- bedside echocardiography shows some promise for monitoring and titrating therapy
- CNS Dysfunction
- Definition and Management
- defined by the Glasgow coma scale
- clinical presentation may range from delirium to coma
- besides the brain injury resulting from MODS, the neurologic system is also affected
by premorbid dementia, substance abuse, pain, altered sleep-wake cycles in the ICU,
and medications
- Haldol is the most efficacious drug for delirium, and benzodiazepines must be
avoided
- sitters, minimizing restraints, and transferring out of the ICU if possible are
additional management strategies to consider
- Nutrition in MODS
- early enteral nutrition improves outcomes in patients with MODS
- calories and protein requirements are titrated to the underlying disease process, with trauma and
burn patients requiring the highest calories and protein
- glutamine supports the gut mucosa and improves outcomes in MODS
- omega-3 fatty acids support immune function and reduce infectious complications
- vitamins and minerals (zinc, selenium, vitamin C and folate) must be supplemented to support wound
healing and immune function
References
- Schwartz, 10th ed., pgs 109 – 131
- Cameron, 13th ed., pgs 1426 - 1432, 1432 - 1439
- UpToDate. Evaluation and Management of Suspected Sepsis and Septic Shock in Adults. Schmidt, Gregory.
Aug 18, 2021, Pgs 1 - 55.
- UpToDate. Sepsis Syndromes in Adults: Epidemiology, Definitions, Clinical Presentation, Diagnosis, and
Prognosis. Neviere, Remi. Aug 25, 2021, Pgs 1 – 42.
- Sepsis 2018: Definitions and Guideline Changes. Napolitano, Lisa. Surgical Infections, Volume 19,
Number 2, 2018. Pgs 117 - 125