Gastroesophageal Reflux Disease (GERD)
- Pathophysiology
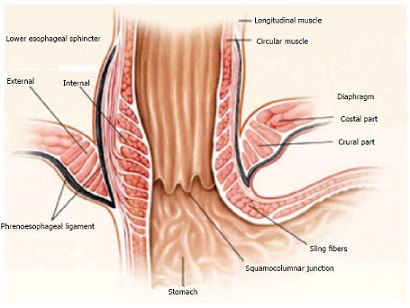
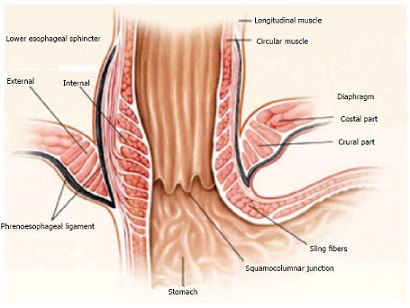
- Lower Esophageal Sphincter (LES) Physiology
- not a distinct anatomic structure, but rather a high pressure zone
- muscles of the distal esophagus are tonically contracted, and relax when a swallow is initiated
- sling fibers of the gastric cardia, which are at the same depth as the circular muscle fibers of the
esophagus but are oriented in a different direction, also contributes to the esophageal high-pressure zone
- the diaphragm contributes to LES pressure by compressing the esophagus when it contracts
- positive intraabdominal pressure also contributes to LES pressure
- Decreased LES Pressure
- Transient Loss of LES Pressure
- LES is structurally normal
- responsible for ‘physiologic’ reflux
- results from gastric distention secondary to overeating,
stress aerophagia, delayed gastric emptying, increased intragastric or increased intraabdominal pressure
- gastric distention pulls open the LES and reduces its overall length
- when a critical length is reached, between 1 and 2 cm, LES pressure drops markedly and reflux occurs
- after gastric venting occurs, sphincter length is restored and competence returns until further distention
again shortens the LES
- Permanent Loss of LES Pressure
- results from structural damage to the components of the LES: loss of pressure, inadequate overall length, or loss of abdominal length
- reduced LES pressure is most likely due to an abnormality of myogenic function (length and tension properties of the LES’s
smooth muscle)
- the efficacy of a LES with normal pressure can be nullified by an inadequate abdominal length or overall length
- an adequate abdominal length is important in preventing reflux caused by increases in intraabdominal pressure
(exertion or changes in body position)
- an adequate overall length is important in preventing reflux caused by gastric distention
- Ineffective Esophageal Clearance
- an effective esophageal pump clears the esophagus of physiologic reflux
- four factors are important in esophageal clearance of gastric juice: gravity,
esophageal motor activity, salivation, and anchoring of the distal esophagus in the abdomen (hiatal hernia)
- ineffective esophageal clearance is usually seen in association with a structurally defective LES, which augments
the esophageal exposure to gastric juice by prolonging the duration of each reflux episode
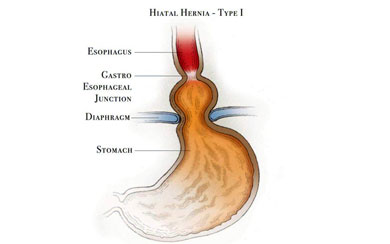
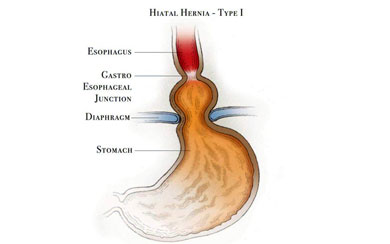
- Hiatal Hernia
- sliding (type I) is the most common hiatal hernia associated with reflux
- occurs when the phrenoesophageal ligament does not maintain the GEJ in the abdominal cavity
- there is a strong association between GERD and hiatal hernia: most patients with GERD have a hiatal hernia, and
the larger the hernia the greater the amount of acid reflux
- however, not every patient with reflux has a hiatal hernia; and not every patient with a hiatal hernia has reflux
- Clinical Presentation
- Symptoms
- most common symptoms are substernal heartburn (early) and acid regurgitation (late)
- however, these symptoms are very common in the general population and may be caused by many other
diseases besides GERD
- also, GERD may present with atypical symptoms such as nausea, vomiting, postprandial fullness,
chest pain, chronic cough, wheezing, asthma, or recurrent pneumonia
- using clinical criteria alone to define GERD lacks sensitivity and specificity
- to make the diagnosis of GERD, objective evidence is required (endoscopy, pH probe, Barrett’s esophagus)
- Complications of GERD
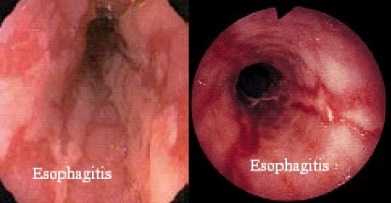
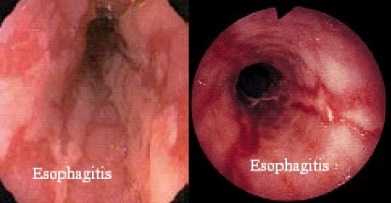
- Esophagitis
- repeated injury and repair leads to fibrosis and progressive deterioration of esophageal contractility
- stricture and Barrett’s esophagus are the end stages of chronic esophagitis
- Stricture
- most common symptom is dysphagia
- need to rule out tumor, motor disorder, diverticula
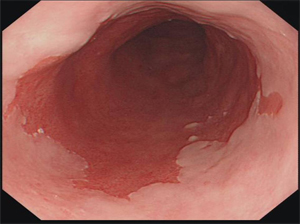
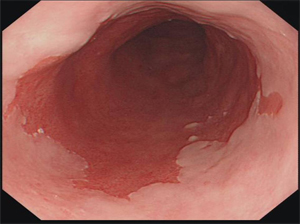
- Barrett’s Esophagus
- defined as the pathological replacement of the esophagus’ normal
stratified squamous epithelium with an intestinal-like columnar epithelium (intestinal metaplasia)
- caused by chronic esophageal injury and inflammation
- represents an increased risk of developing esophageal adenocarcinoma (0.5% per year)
- Aspiration
- refluxed gastric juice can reach the pharynx
- symptoms include repetitive cough, choking, hoarseness, and recurrent pneumonia
- GERD may be responsible for pulmonary diseases such as asthma, pulmonary fibrosis, and bronchiectasis
- Treatment of GERD
- Empiric Medical Management
- patients with symptoms of heartburn without obvious complications can be given a 6 week trial of a proton pump
inhibitor (PPI) without further studies
- additional lifestyle interventions include elevating the head of the bed, avoiding tight clothing, eating small,
frequent meals, avoiding eating shortly before bed, losing weight, and avoiding alcohol, coffee and chocolate
- most patients (80%) have a recurrence of GERD after discontinuation of any type of medical therapy
- long-term complications of PPIs are being studied: nutritional deficiencies, infectious complications, gastric polyp formation,
osteoporosis
- Evaluation
- required for all patients being considered for surgery, as well as for patients with atypical symptoms or
possible complications
- Endoscopy
- very high specificity for diagnosing GERD, but lacks sensitivity – about 50% of GERD patients have normal
endoscopic findings
- severity of symptoms correlates poorly with the severity of esophagitis
- most useful for detecting complications of GERD (erosive esophagitis, Barrett’s metaplasia) and excluding other
diseases (cancer, stricture)
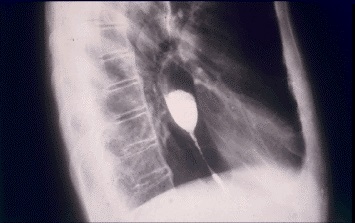
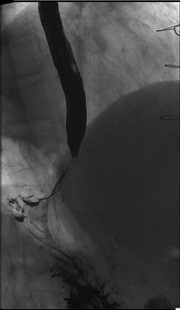
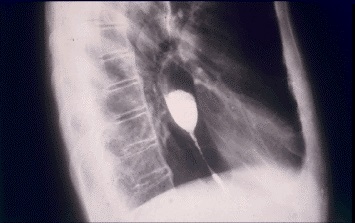
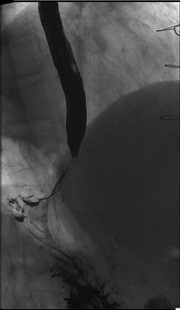
- Esophagram
- provides valuable information about the external anatomy of the stomach and esophagus
- provides information about the size and type of hiatal hernia that is present
- may show a ‘short’ esophagus
- Manometry
- if dysphagia or chest pain is present, then manometry is required to exclude an esophageal motility disorder
- fully assesses the adequacy of esophageal contractions
- findings may alter the surgical approach – patients who have weak peristalsis may need a partial fundoplication
instead of a complete wrap
- pH Monitoring
- gold standard for diagnosing and quantifying acid reflux
- allows symptoms to be correlated with reflux events
- patients need to discontinue PPIs one week before the test
- Operative Indications
- ideal candidate for an antireflux operation is a patient who responds well to
medical therapy but is unwilling or unable to continue the medicines (side effects, cost)
- severe esophagitis on endoscopy
- benign strictures
- Barrett’s metaplasia without untreated high-grade dysplasia
- since GERD requires lifelong medical therapy, surgery in younger patients is the more cost effective option
- absolute contraindications are esophageal cancer or Barrett’s esophagus with untreated high-grade dysplasia
- obesity is a relative contraindication, and these patients may benefit more from an obesity operation than a
fundoplication
- Principles of Surgical Treatment of GERD
- procedure chosen should restore the functional and mechanical competence of the LES, reconstruct the hiatus,
and repair any hiatal hernia if present
- must preserve the ability to swallow normally, and belch and vomit as necessary
- the following principles should be adhered to:
- restore the pressure in the LES to twice resting gastric pressure
- restore an adequate length of the LES to the positive-pressure environment of the abdomen (2.5 cm)
- allow the reconstructed cardia to relax on swallowing by avoiding injury to the vagus nerve and only using
the fundus for the wrap
- the fundoplication should not increase the resistance of the relaxed sphincter to a level that exceeds the
peristaltic power of the esophagus
- 360° wrap should be no longer than 2 cm and constructed over a 56 - 60 Fr bougie
- the fundoplication must be placed in the abdomen without undue tension and maintained there by approximating
the crura of the diaphragm above the repair
- Procedure Selection
- laparoscopic transabdominal approach is the preferred approach for most patients
- open transabdominal approach is reserved for patients who require a revisional reflux procedure, or who
have had multiple previous abdominal procedures, or any contraindication to laparoscopy
- transthoracic approach is used when a long esophageal myotomy is required for a primary motility disorder
- complete 360° wrap (Nissen)is preferred for most patients
- partial wraps (Toupet, Dor) are used when there is poor esophageal contractility
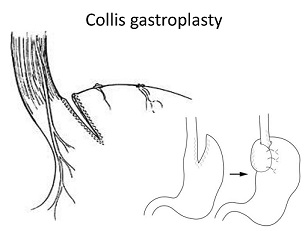
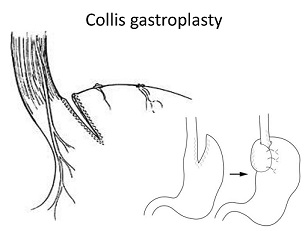
- a short esophagus will require extensive mediastinal mobilization and/or an esophageal lengthening
procedure (Collis Gastroplasty)
- Nissen Fundoplication
- important technical points include:
- retraction of the left lateral lobe of the liver
- identify and expose both crus
- divide the short gastrics
- identify and preserve both vagus nerves
- circumferential mobilization of the esophagus
- crural closure, but too tight can lead to dysphagia
- fundus is passed posterior to stomach, and a short wrap is created over a 56 – 60 Fr bougie

- some series report 90% of patients are symptom-free at 10 years
- Complications
- Esophageal or Gastric Perforation
- endoscopy at the end of the procedure may help to identify this problem
- post-op, patients with unexplained fever or tachycardia should have an UGI
to exclude a perforation or herniated wrap
- Dysphagia
- very common postop problem that usually resolves within several weeks
- persistent symptoms should be evaluated with an UGI
- if the wrap is too tight, serial endoscopic dilations usually resolves the problem
- occasionally, revision of the fundoplication to a partial fundoplication will be necessary
- Gas Bloat Syndrome
- abdominal pain, inability to belch
- caused by air trapping in the stomach
- creation of a short, floppy wrap will usually avoid this problem
- KUB shows a gas-filled stomach
- NG tube decompression immediately alleviates the symptoms
- dietary modifications and prokinetic agents are occasionally helpful,
but some patients will require conversion of their full wrap to a partial wrap
- a pyloroplasty may also benefit some patients with poor gastric emptying
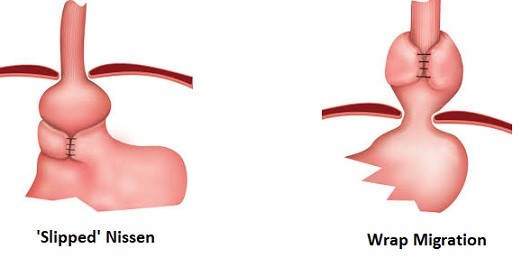
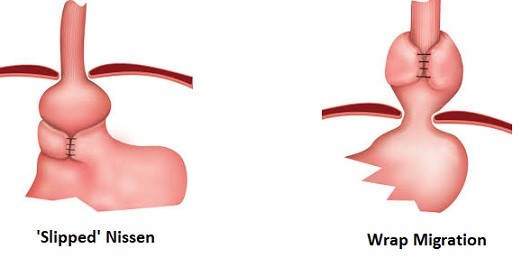
- Slipped or Misplaced Wraps
- if improperly secured to the esophagus, the wrap can slip down onto the body of the stomach,
leading to recurrent reflux symptoms or obstruction
- the wrap may also migrate into the thorax, leading to recurrence of reflux symptoms
- Partial Fundoplications
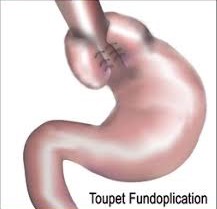
- Toupet Procedure
- 270° posterior wrap
- used for patients with documented esophageal motor abnormalities
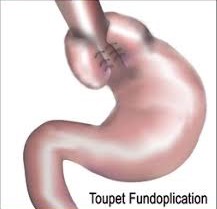
- Dor Procedure
- 180° anterior wrap
- similar indications and results as the Toupet procedure
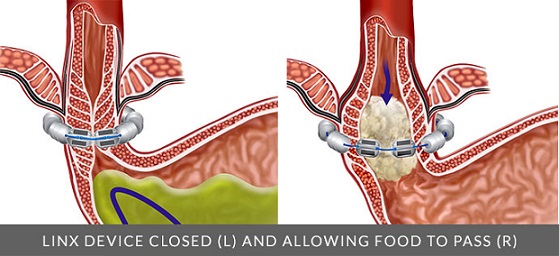
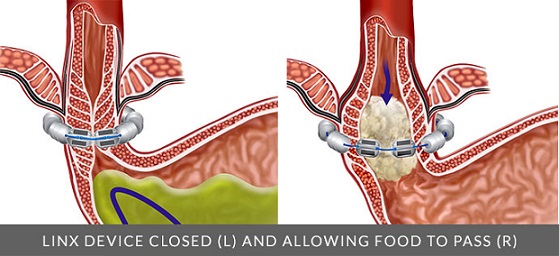
- LINX Prosthesis
- approved by the FDA in 2012
- surgically placed magnetic ring that augments the LES closure pressure but permits food passage
with swallowing
- contraindications include a large hiatal hernia or severe esophagitis
- short term follow-up suggests results similar to laparoscopic fundoplication, but 10 – 20 year
follow up data is not available yet
- some devices have been explanted secondary to dysphagia or esophageal erosion
- older devices are not MRI-compatible; new devices are MRI-conditional
- Endoscopic Approaches
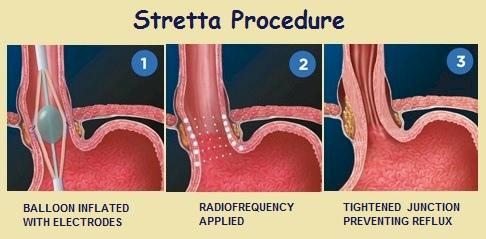
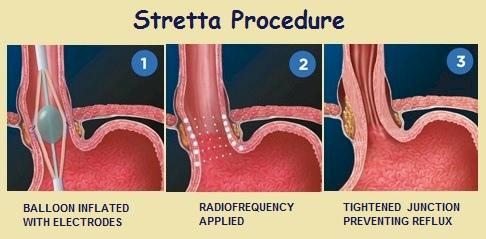
- Stretta Procedure
- radiofrequency energy is applied to the muscle of the LES and gastric cardia,
strengthening and thickening the muscle
- must have an LES pressure ≥ 8 mm Hg and a hiatal hernia < 3 cm long to be eligible
for the procedure
- Transoral Incisionless Fundoplication (Esophyx)
- full-thickness serosa-to-serosa plication that is 3 – 5 cm in length and 200 – 300 degrees in circumference
- questions remain about the long-term durability of the procedure

References
- Sabiston, 19th ed., pgs 1033 – 1036, 1067 – 1083
- Cameron, 11th ed., pgs 9 – 14, 19 – 23, 27 – 36
- UpToDate. Clinical manifestations and Diagnosis of Gastroesophageal Reflux in Adults. Kahrilas MD, Peter. March 2018. Pgs 1 – 21
- UpToDate. Surgical Management of Gastroesophageal Reflux in Adults. Schwaitzberg MD, Steven. Jan 02, 2019. Pgs 1 – 35