Esophageal Motility Disorders
Achalasia
- Pathophysiology
- ‘lack of relaxation’
- results from degeneration of ganglion cells in the myenteric plexuses of the esophageal wall,
which may be idiopathic (most common) or infectious (Chagas’ disease)
- the neurons that are primarily affected are inhibitory, resulting in unopposed smooth muscle stimulation and,
ultimately, failure of relaxation of the LES and aperistalsis
- hypertension of the LES leads secondarily to elevated esophageal pressure and esophageal dilatation
- some achalasia patients also have a defect in UES relaxation, leading to loss of the belch reflex
- premalignant condition (8% chance of developing cancer at 20 years)
- Presentation
- dysphagia for both solids and liquids that develops over many years
- regurgitation of undigested food
- use of large quantities of water to wash food down
- GERD-like retrosternal burning pain
- aspiration pneumonia common
- Diagnosis
- Barium Esophagram
- mild dilatation early, massive dilatation (megaesophagus) late
- peristalsis disordered early, nonexistent late
- retained intraesophageal contents typical
- classic finding is the ‘bird’s beak’ taper

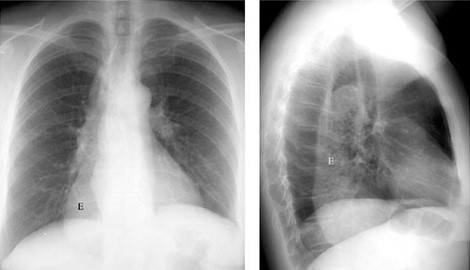
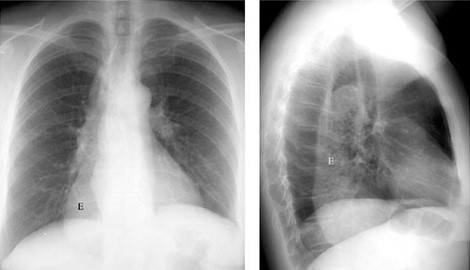
- Chest X-ray
- widened mediastinum
- posterior mediastinal air-fluid level
- absence of gastric air bubble
- Manometry
- gold standard test for diagnosis
- incomplete LES relaxation with swallowing
- elevated LES pressure (> 35 mm Hg)
- increased intraesophageal baseline pressure
- aperistalsis in the esophageal body
- low-amplitude waveforms indicating a lack of muscular tone
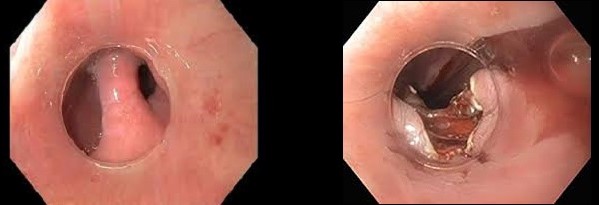
- Esophagoscopy
- useful to evaluate for esophagitis or the presence of carcinoma
- Therapy
- palliative, not curative
- treatment directed towards relieving the obstruction caused by a nonrelaxing LES
- no treatment addresses the decreased motility in the esophageal body
- Medical Therapy
- sublingual nitroglycerin, nitrates and calcium-channel blockers may help alleviate symptoms very early in
the disease, or in patients who are not candidates for more invasive treatments
- least effective treatment option
- Botulinum Toxin Therapy (Botox)
- injected directly into the LES during endoscopy
- most patients have early improvement in symptoms but require retreatment within 6 – 12 month
- Esophageal Dilatation
- hydrostatic or pneumatic balloons are used to dilate and rupture the fibers of the LES
- multiple endoscopies are required per treatment (graded approach)
- initial success rates are high (85%), but efficacy wanes over time
- main complication is esophageal rupture (4%) which has a 20% mortality rate
- procedure may be repeated when symptoms recur, but each subsequent dilation is progressively less
likely to result in a sustained remission
- often is the first treatment chosen
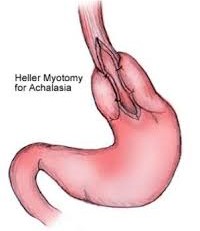
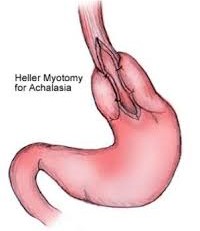
- Surgical Therapy
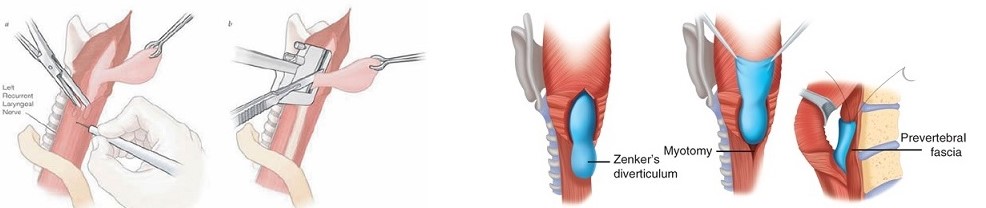
- esophageal myotomy is needed to relieve LES hypertension
- classic approach is the transthoracic left-sided open myotomy from the gastric cardia to the level of
the aortic arch
- procedure can also be done from a transabdominal approach
- laparoscopic and thoracoscopic approaches are now becoming standard
- an area of controversy is whether an anti-reflux procedure is necessary and which procedure should be done
- a complete 360-degree Nissen fundoplication has the potential to increase LES pressure and worsen symptoms of
esophageal obstruction - for this reason, a partial wrap (Toupet) is often chosen
- esophagectomy (transhiatal) should be considered for end-stage disease or failure of more than one myotomy
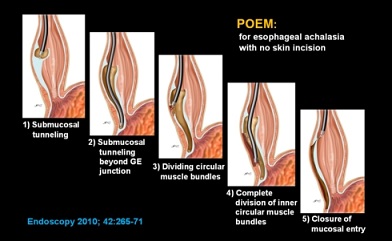
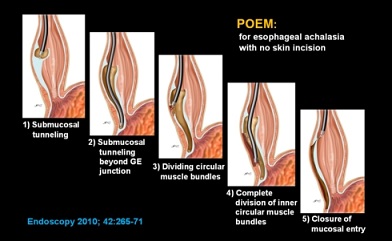
- Per-Oral Endoscopic Myotomy
- replicates the surgical procedure endoscopically
- no long-term follow up data yet
Distal (Diffuse) Esophageal Spasm
- Pathophysiology
- poorly understood hypermotility disorder
- motor abnormality of the lower two-thirds of the esophagus that may be related to impaired inhibitory innervation
- muscular hypertrophy and degeneration of branches of the vagus nerve have been observed
- esophageal contractions are repetitive, simultaneous, high-amplitude, tertiary
- Presentation
- chest pain, often mimicking angina pectoris by radiating into the neck or down the arm
- dysphagia for solids and liquids is common
- regurgitation of food is unusual
- may have other functional GI disorders (irritable bowel syndrome, pyloric spasm)
- Diagnosis
- initial evaluation usually is cardiac in nature (chest x-ray, EKG)
- esophageal etiology is often considered only after a negative cardiac workup
- need also to rule out intraabdominal pathology (gallstones, peptic ulcer)
- esophagoscopy is necessary to rule out a distal obstructing lesion that produces tertiary
contractions
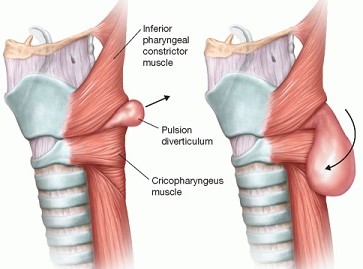
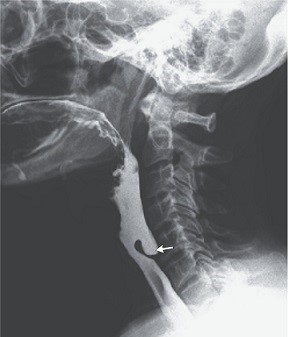
- barium esophagram may show a thickened esophageal wall (>5 mm), pulsion diverticulum, the classic ‘corkscrew’ esophagus,
or it may be normal

- manometry is the critical diagnostic test
- repetitive, simultaneous, high-amplitude or long duration tertiary contractions define spasm
- if standard or ambulatory manometry fails to demonstrate DES, provocative maneuvers (bethanecol) may induce
the motility disorder
- diagnostic goal is the correlation of subjective symptoms with objective evidence of spasm on manometry
- Treatment
- Medical Therapy
- avoid ‘trigger’ foods
- control GERD symptoms with PPIs
- antispasmodics are occasionally helpful (peppermint oil – Altoid mints)
- calcium channel blockers or nitroglycerine are occasionally helpful
- tricyclic antidepressants are helpful for some patients
- Endoscopic Therapy
- bougie dilation for severe dysphagia provides relief in 70% - 80%
- Botox injections may provide short-term relief
- Surgical Therapy
- results are much less favorable than in achalasia
- esophagomyotomy should be used only in the most severe and refractory cases of dysphagia, or if a pulsion
diverticulum is present
- a long transthoracic myotomy is necessary, extending from the aortic arch onto the proximal stomach
- since the myotomy will make the LES incompetent, an anti-reflux procedure is necessary
- a 360-degree fundoplication is contraindicated, just as in the case in achalasia
Hypercontractile (Nutcracker) Esophagus
- Presentation
- symptoms are similar to DES: chest pain, dysphagia, odynophagia
- most painful of all esophageal hypermotility disorders
- Diagnosis
- barium swallow may show segmental spasm, or be normal
- manometry shows extremely high-amplitude (225 to 430 mm Hg) normally progressive peristaltic contractions, often of prolonged duration (> 6 seconds)
- LES pressure is normal and relaxes with each wet swallow
- manometry findings need to coincide with subjective complaint of chest pain
- ambulatory monitoring may be necessary to distinguish this disorder from DES
- Therapy
- medical management is the treatment of choice and is similar to the management of DES
- avoid trigger foods
- surgery rarely is indicated or helpful
Ineffective Esophageal Motility
- Pathophysiology
- contraction abnormality of the distal esophagus
- usually associated with GERD
- may be secondary to inflammatory injury to the esophageal body
- decreased motility of the esophageal body leads to poor acid clearance in the lower esophagus
- Symptoms
- reflux symptoms and dysphagia
- Diagnosis
- esophagram shows nonspecific abnormalities of esophageal contraction
- diagnosis made by manometry: nontransmitted or low-amplitude peristaltic contractions in more than
30% of wet swallows, decreased LES tone
- Treatment
- altered motility is irreversible
- best treatment is prevention: effective treatment of GERD
References
- Sabiston, 19th ed., pgs 1023 – 1032
- Cameron, 11th ed., pgs 39 – 43, 44 – 47
- UpToDate. Zenker’s Diverticulum. Schiff MD, Bradley. May 28, 2019. Pgs 1 – 22
- UpToDate. Achalasia: Pathogenesis, Clinical Manifestations, and Diagnosis. Spechler MD, Stuart. Feb 09, 2018. Pgs 1 – 22
- UpToDate. Overview of the Treatment of Achalasia. Spechler MD, Stuart. March 15, 2019. Pgs 1 – 17
- UpToDate. Major Disorders of Esophageal Hyperperistalsis: Clinical Features, Diagnosis, and Management. Castell MD, Donald. July 17, 2019. Pgs 1 – 21