Gallbladder and Bile Duct Anatomy and Physiology
Anatomy
- Gallbladder
- pear-shaped organ located in the bed of the liver
- average capacity is 30 to 50 ml
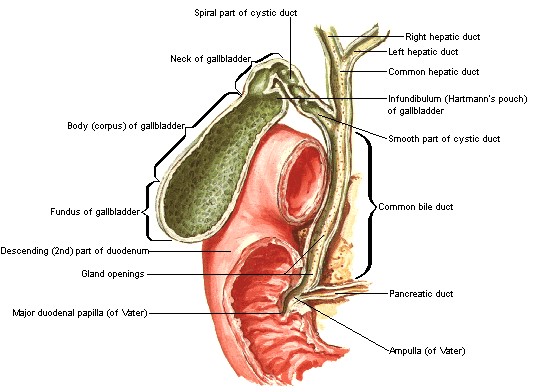
- divided into 4 anatomic portions: fundus, body, infundibulum, and neck
- wall of the gallbladder is made up of smooth muscle and fibrous tissue
- lumen is lined by a high columnar epithelium
- lacks a muscularis mucosa and submucosa
- Cystic Duct
- connects the gallbladder with the common bile duct
- usually 2 to 4 cm long
- contains the spiral valves of Heister, which allow easy entry of bile into the gallbladder
but resist its outflow
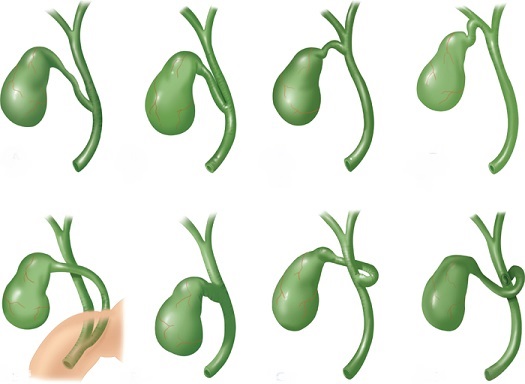
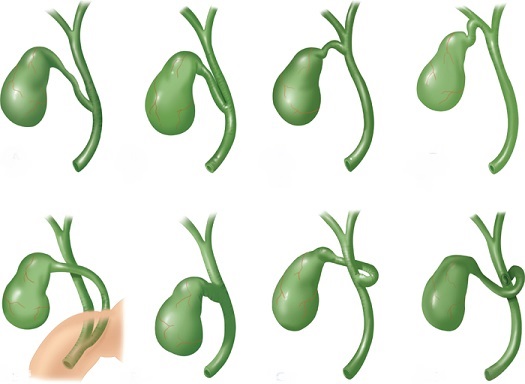
- Anatomic Variations
- point of union of the cystic duct with the common hepatic duct is extremely variable
- the cystic duct may enter the hepatic duct high or low, it may be adherent to the
common hepatic duct, it may be very short or absent, it may join the right hepatic duct,
or it may course underneath the common hepatic duct and enter it posteriorly
or on its left side
- accessory ducts from the liver may enter the cystic duct or common hepatic duct
- small ducts (of Luschka) may drain directly from the liver into the gallbladder
- knowledge of these common variations is important in order to avoid iatrogenic injury
during cholecystectomy
- Blood Supply, Lymphatic Drainage, and Nerve Supply
- the cystic artery originates from the right hepatic artery (90%) and has an anterior and
posterior branch
- venous drainage is into the portal vein
- lymphatic drainage is into the cystic duct node
- hepatic branch of the vagus nerve supplies parasympathetic fibers
- pain of biliary colic is mediated by sympathetic afferent fibers
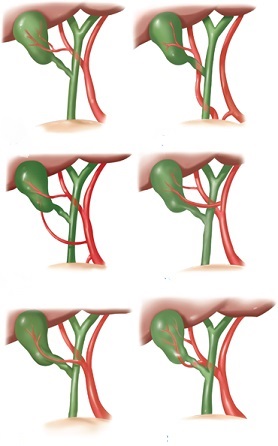
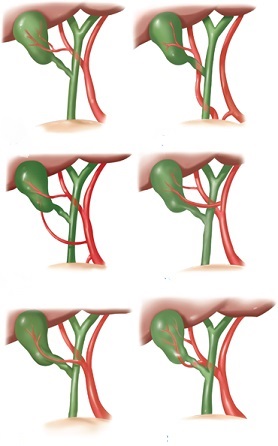
- Cystic Artery Variations
- in 20% of cases, the right hepatic artery comes off the SMA
- in 5% of the cases, there are 2 right hepatic arteries
- since the right hepatic artery is variable in location, the cystic artery can also
be in variable locations
- rarely, the cystic artery may arise from a different artery than the right hepatic
- Biliary Tree
- extrahepatic bile ducts are located within the hepatoduodenal ligament
- right hepatic duct is formed by the union of the right anterior and posterior segmental ducts;
left hepatic duct is formed by the union of the left lateral and left medial segmental ducts
- the left hepatic duct is longer than the right and a greater portion of it is extrahepatic since it
follows a more transverse course to the liver
- common hepatic duct is formed by the union of the left and right hepatic ducts
- length of the common hepatic duct is variable since this is dependent on where the cystic duct joins it
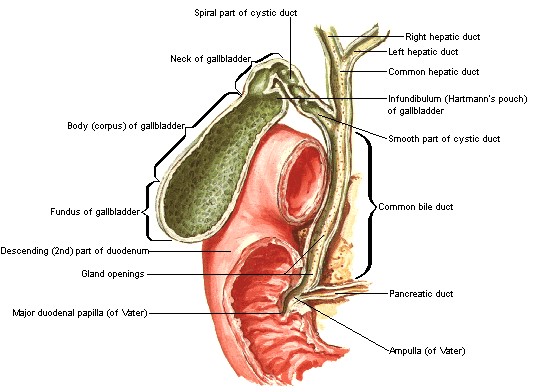
- Common Bile Duct
- formed by the union of the cystic duct and common hepatic ducts
- located to the right of the hepatic artery and anterior to the portal vein in the
hepatoduodenal ligament
- blood supply is via two axial vessels, the 3 o’clock and 9 o’clock arteries
- travels through the pancreas and the wall of the duodenum to form the papilla of Vater
- its distal end is surrounded by the sphincter of Oddi, which regulates the flow of bile
into the duodenum
- pancreatic duct may share a common orifice on the papilla of Vater with the common bile duct,
it may join the common duct proximal to its entrance into the duodenum, or the two ducts may
open separately on the papilla
Physiology
- Bile Function
- route of excretion for certain organic solutes (bilirubin, cholesterol)
- facilitates absorption of lipids and fat-soluble vitamins
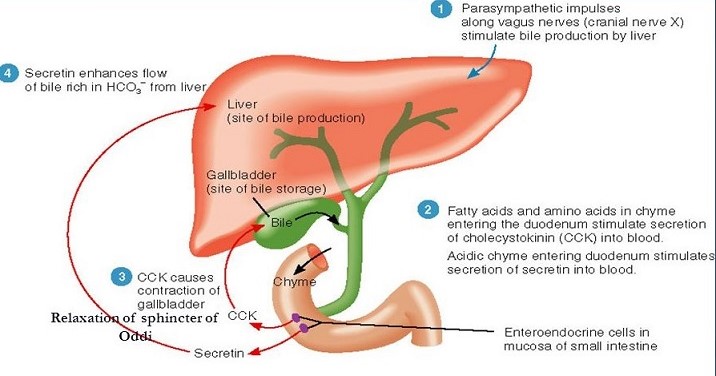
- Bile Formation and Secretion
- ~1000 ml/day of bile is produced by the hepatocytes
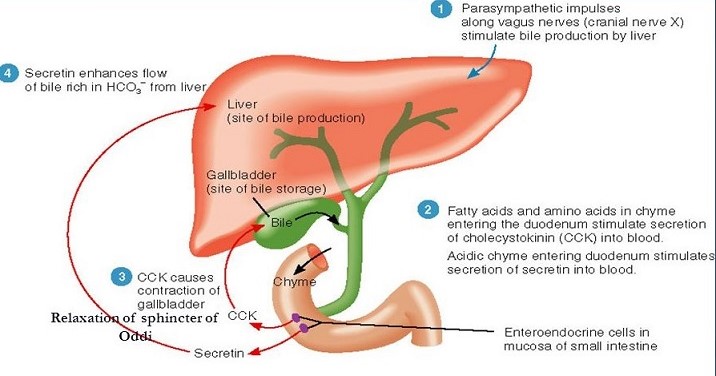
- rate of secretion is under neurogenic, humoral, and chemical control
- vagal stimulation increases bile flow; sympathetic splanchnic stimulation decreases bile flow by decreasing
hepatic blood flow
- gastrointestinal hormones such as secretin, cholecystokinin, gastrin, and glucagon all increase
bile flow, primarily by increasing water and electrolyte secretion from duct cells
- most important factor in regulating the volume of bile secretion is the rate of bile salt secretion,
which in turn is regulated by the return of bile salts to the liver from the enterohepatic circulation
- Bile Composition
- water constitutes 85% of the volume of bile
- the major organic solutes of bile are bile salts, bilirubin, phospholipids, and cholesterol
- Bile Salts
- steroid molecules synthesized from cholesterol in the liver
- amphipathic compounds, containing both a hydrophobic and a hydrophilic portion
- 2 primary bile salts, cholic and chenodeoxycholic acid
- the primary bile salts are conjugated with either taurine or glycine
- primary bile salts may then undergo chemical alteration in the intestine to form
secondary bile salts (deoxycholate and lithocholate)
- purpose of bile salts is to solubilize lipids and facilitate their absorption
- Bilirubin
- breakdown product of hemoglobin excreted almost entirely in bile
- conjugated in the liver with glucuronide
- in the intestine, bilirubin is converted into urobilinogen and excreted in the stool
- Phospholipids
- lecithin is the primary phospholipid in bile
- Micelle Formation
- cholesterol is highly nonpolar and thus insoluble in water (and bile)
- micelles, a bile salt-phospholipid-cholesterol complex, are the keys to maintaining cholesterol in solution
- in aqueous solutions, bile salts are oriented with their hydrophilic portion outwards
- phospholipids are incorporated into the micellar structure, allowing cholesterol to be added to the
hydrophobic central portion of the micelle
- in this way, cholesterol can be maintained in an aqueous environment
- however, cholesterol solubility depends on the relative concentrations of cholesterol, bile salts,
and lecithin - any changes in these relative concentrations can alter the ability of the micelle to
keep cholesterol in solution
- Gallbladder Function
- main function is to store and concentrate hepatic bile during the fasting state, allowing for a
coordinated response to a meal
- Storage and Absorption
- gallbladder mucosa has the greatest absorptive capacity per unit area of any structure in the body
- bile is usually concentrated 5-fold to 10-fold by the active transport of sodium and the
passive transport of water
- this absorptive ability of the gallbladder allows the small capacity gallbladder (30 to 50 ml)
to store the large output (1000ml/day) of bile from the liver
- Secretion
- glands of the gallbladder neck and cystic duct secrete mucus glycoproteins
- mucus layer protects the gallbladder epithelium from the strong detergent effect of the highly
concentrated bile salts
- responsible for the ‘white bile’ present in hydrops of the gallbladder
- Motility
- gallbladder filling occurs because the resting pressure in the common bile duct is greater
than in the gallbladder (tonic contraction of the sphincter of Oddi)
- passage of bile into the duodenum involves the coordinated contraction of the gallbladder and
relaxation of the sphincter of Oddi, which is largely mediated by the release of CCK from the
duodenum after the ingestion of food
- emptying of the gallbladder takes place 30 minutes after ingestion of a fatty meal
- between meals, the gallbladder empties ~ 10% to 15% of its volume with each passage through the
duodenum of the MMC (this process is mediated in part by motilin)
- defects in gallbladder motility, which increase the length of time of bile in the gallbladder,
play a role in the pathogenesis of gallstones
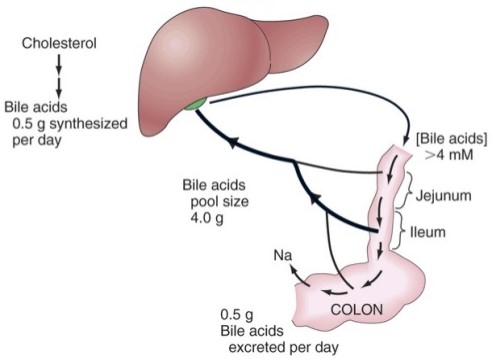
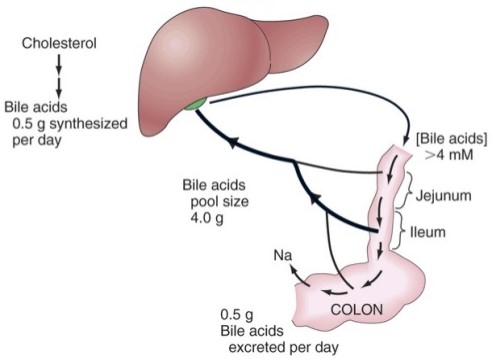
- Enterohepatic Circulation
- 80% of conjugated bile salts are absorbed in the terminal ileum
- majority of the rest are deconjugated by bacterial activity and absorbed by the colon
- ultimately, 95% of the bile salts are reabsorbed and returned to the liver via the portal vein
- 5% of the bile salt pool is lost each day in the stool and must be resynthesized by the liver
- in cases of ileal resection or biliary fistula, bile salt production by the liver is increased to
maintain a normal bile salt pool
References
- Schwartz, 10th ed., pgs 1309 - 1316
- Sabiston, 20th ed., pgs 1482 - 1486
- O’Leary, pgs 450 - 452