Ventral and Incisional Hernias
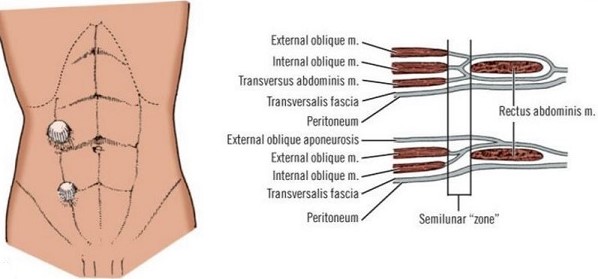
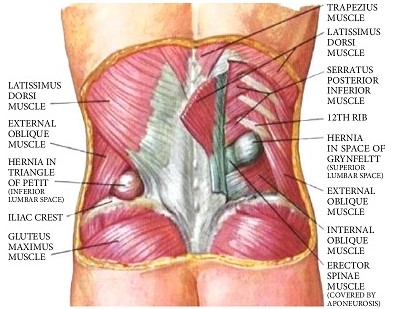
Anatomy of the Abdominal Wall
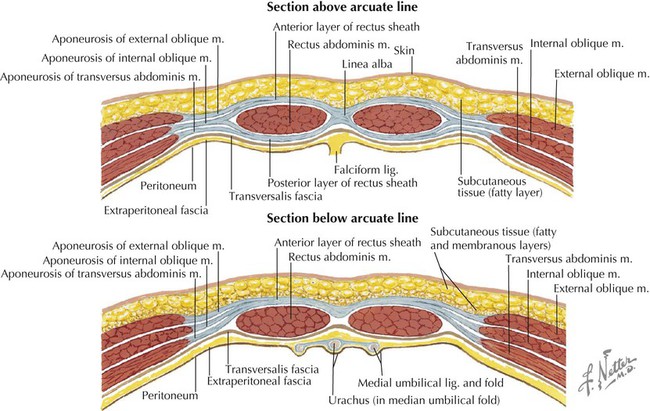
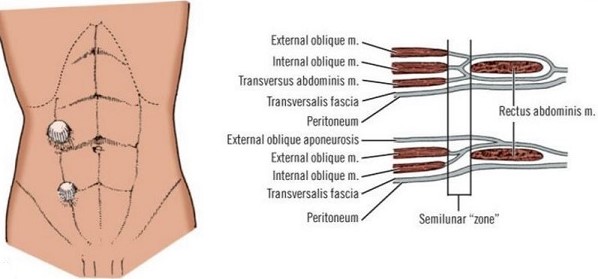
- Muscle Layers
- Rectus Muscles
- longitudinally paired muscles encased within fascial sheaths
- the linea alba is where the anterior and posterior fascial sheaths fuse at the midline
- the arcuate line lies at roughly the level of the anterior superior iliac spine
- above the arcuate line, the posterior rectus sheath is made up of the internal lamina of the internal
oblique fascia and the transverse abdominis fascia
- below the arcuate line, the posterior rectus sheath is absent
- laterally, the rectus sheath fuses with the fascia of the lateral muscles to form the semilunar line
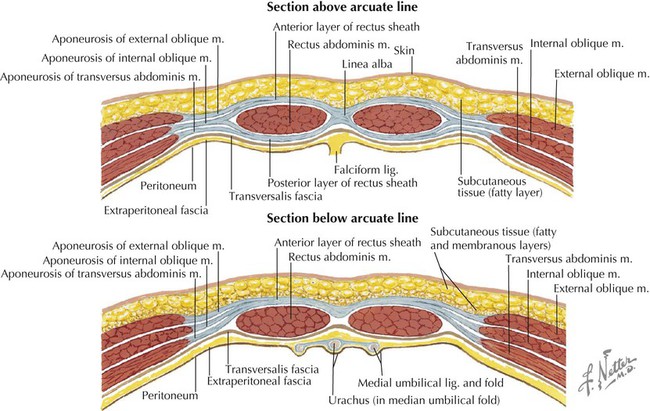
- Lateral Muscles
- 3 muscles oriented obliquely to each other
- the fascia of these layers combine to form the semilunar line, which then contributes to the
anterior and posterior rectus sheaths
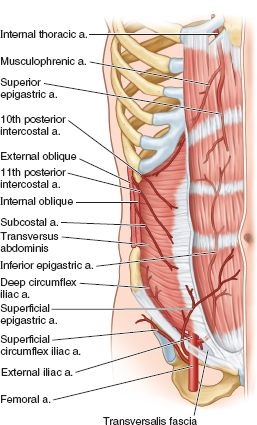
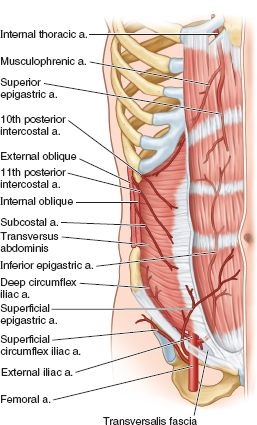
- Blood Supply
- primarily originates from the superior and inferior epigastric arteries
- inferior epigastric artery originates from the external iliac artery
- superior epigastric artery originates from the internal thoracic artery
- a collateral network of intercostal, lumbar, and deep circumflex iliac arteries also
contributes to abdominal wall blood supply
Ventral Hernias
- Umbilical Hernias
- Etiology
- Children
- congenital in origin
- most close spontaneously by age 2
- 8X more common in African-Americans
- Adults
- acquired condition
- more common in women
- may result from conditions that increase intra-abdominal pressure: pregnancy, obesity,
ascites, constipation, chronic cough
- Management
- small, asymptomatic hernias do not need to be repaired
- all symptomatic hernias should be repaired
- defects < 3 cm in size can often be close primarily after excising the hernia sac
- larger defects are closed with a mesh patch placed in an inlay, onlay, or sublay position
- repairs may be done open or laparoscopically
- no universal consensus on the best method of repair
- Umbilical Hernia Repair in Cirrhotics
- umbilical hernias in patients with ascites will continue to enlarge
- skin breakdown with spontaneous rupture of the hernia can result in peritonitis and death
- cirrhotics are often hypoalbuminemic and coagulopathic, making them high-risk surgical candidates
- historically, elective repair was contraindicated because of the high morbidity and mortality rates
- with modern preoperative and intraoperative management, serious complication rates are < 10%,
making elective repair feasible for many patients

- Preoperative Preparation
- includes free water restriction, diuretics, and large volume paracenteses
(with infusion of albumin)
- some series report good results with perioperative placement of a temporary peritoneal dialysis catheter or
transjugular intrahepatic portosystemic shunt
- there is no current indication for placement of a perioperative peritoneovenous shunt
- Surgical Management
- use of synthetic mesh is not contraindicated, and is associated with lower recurrence
rates (3%) than primary repairs (15%)
- both onlay and retrorectus sublay repairs give equivalent results
- venous abdominal wall collaterals should not be ligated because this can cause hepatic
decompensation
- Epigastric Hernias
- Presentation
- more common in men
- located between the xiphoid process and the umbilicus
- usually are painful because they often contain incarcerated preperitoneal fat
- Management
- repair is indicated, since most are symptomatic
- small hernias can be closed primarily, but larger lesions will require mesh
- Diastasis Recti
- may be confused with an epigastric hernia
- is an area of weakness that results from the stretching of the linea alba
- presents as a diffuse midline bulge, but no true hernia defect is present
- abdominal US or CT scan can confirm the diagnosis
- does not require repair
- Incisional Hernias
- Etiology
- result from excessive tension and inadequate healing of an incision
- wound infections and hematomas greatly increase the risk of incisional hernias
- corticosteroids and chemotherapy drugs contribute to poor wound healing
- other risk factors include obesity, older age, malnutrition, ascites, diabetes,
chronic pulmonary disease
- Pathophysiology
- pain, bowel obstruction, incarceration, and strangulation may result
- large hernias may result in loss of abdominal domain
- Nonoperative Management
- preferred option for asymptomatic or mildly symptomatic patients
- symptomatic patients with modifiable risk factors should also initially be managed nonoperatively
- patients with a BMI > 35 should be put on a weight loss program or may need to consider bariatric surgery
before proceeding with hernia surgery
- patients will also need to quit smoking and get their diabetes under good control before considering
elective surgery
- Operative Repair
- almost all will require a mesh repair
- choice of mesh will depend on whether the mesh will be in direct contact with the bowel, and the
presence or risk of infection
- the ideal mesh has yet to be developed
- Types of Mesh
- Polypropylene Mesh (Marlex)
- macroporous mesh that allows ingrowth of fibroblasts and incorporation into the
surrounding fascia
- should not be placed in an intraperitoneal position, since bowel will adhere to it,
resulting in a high rate of enterocutaneous fistulas
- PTFE Mesh (Gortex)
- impermeable to fluid
- not incorporated into native tissue
- resists adhesion formation
- Composite Mesh
- consists of a PTFE surface and a polypropylene surface
- PTFE side is placed against the bowel, and the polypropylene side is placed superficially
and is incorporated into the native tissue
- since these materials have different rates of contraction, buckling of the mesh can occur,
with resulting exposure of the polypropylene surface to the bowel
- Biologic Mesh
- nonsynthetic, natural tissue mesh
- comes from human, bovine, or porcine sources
- composed of acellular collagen
- provides a framework for neovascularization and native collagen deposition
- typically used in infected or contaminated cases in which synthetic mesh is contraindicated
- functions best as a fascial reinforcement rather than as a bridge or interposition repair
- long-term durability of these products is unresolved
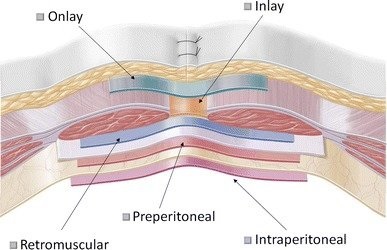
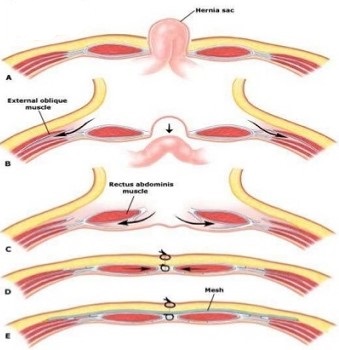
- Mesh Placement
- basic concept is to place a piece of mesh larger than the defect with a wide overlap
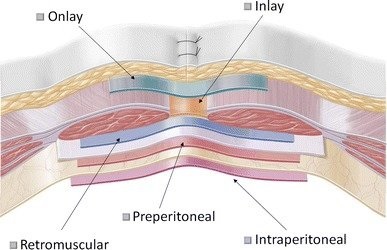
- Overlay Technique
- involves primary closure of the fascial defect (if possible), and placement of the mesh
over the anterior fascia
- major advantage is that the mesh is not in contact with the bowel
- major disadvantages include large subcutaneous flaps, increased seroma formation,
superficial location of the mesh with increased infection risk, and the
increased tension from the primary closure
- reported recurrence rate is ~28%
- Inlay Technique
- involves suturing the mesh to the fascial edges without overlap
- has the highest recurrence rate
- Sublay Technique
- mesh is widely placed below the fascia
- mesh can be placed preperitoneally or retromuscularly
- intra-abdominal pressure will help to hold the mesh in place
- lower recurrence rate and complication rate than the overlay or inlay techniques
- Intraperitoneal Mesh Placement
- laparoscopic repairs use intraperitoneal composite mesh placement secured with tacks or
mattress sutures
- one advantage is the ability to widely place the mesh around the hernia defect
(at least 4 cm)
- associated with fewer wound complications
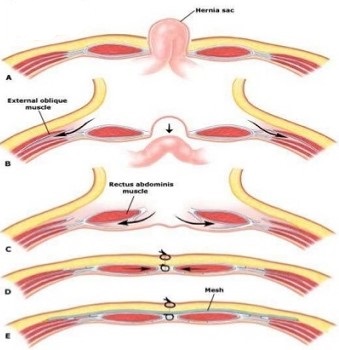
- Components Separation
- used to create an advancement flap of the rectus muscles towards the midline
- usually is augmented with mesh placed in an onlay or sublay position
- restores the linea alba, resulting in a more functional abdominal wall
- Anterior Component Separation
- large subcutaneous flaps are raised above the external oblique fascia
- bilateral longitudinal relaxing incisions are made in the external oblique fascia
2 cm lateral to the semilunar line
- extent of the relaxing incision is from the costal margin to the pubis
- the external oblique is bluntly dissected away from the internal oblique, facilitating
its advancement
- if necessary, additional release may be obtained by making a relaxing incision in the
posterior rectus sheath
- up to 20 cm of mobilization can be obtained with these techniques
- common complication is wound breakdown from devascularized skin flaps caused by the
extensive undermining required
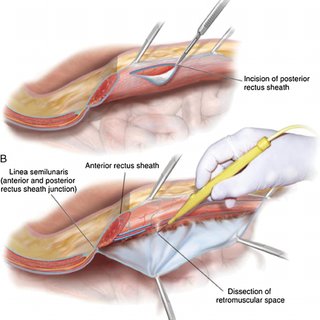
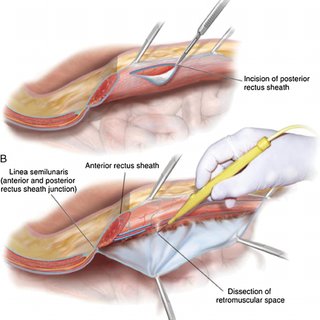
- Transversus Abdominis Release (TAR)
- TAR starts by entering the posterior rectus sheath and developing a retrorectus plane
- the lateral dissection is extended to 1 cm medial to the linea semilunaris preserving the
neurovascular bundles innervating the medial abdominal wall
- the transversus abdominis muscle fibers are identified and divided to enter a retromuscular
and preperitoneal plane
- the dissection is then continued laterally to the psoas muscle
- after bilateral TAR is completed, the posterior rectus sheath is closed in the midline to
fully isolate the visceral contents from prosthetic mesh placement
- closure of the posterior rectus sheath also creates a space for the placement of a large
piece of mesh in a sublay retromuscular position
- after mesh implantation, the rectus muscle and anterior rectus sheath are closed above
the mesh to restore the midline abdominal wall
- Complications
- Mesh Infections
- PTFE mesh will need to be removed
- Marlex mesh can sometimes be salvaged with wound debridement and conservative
excision of unincorporated mesh
- laparoscopic repairs are associated with a much lower incidence of wound complications
- Seromas
- in open repairs, drains are usually placed to obliterate the dead space caused by dissecting
out the hernia sac
- seromas commonly reform after the drains are removed
- drains are also a conduit for bacterial contamination of the mesh
- in laparoscopic repairs, since the hernia sac is not removed, seromas are inevitable
- wearing an abdominal binder 24 hours/day can minimize and prevent seroma formation
- Bowel Injury
- may occur during adhesiolysis
- management depends on the type of bowel injured (small bowel vs colon), and the amount of spillage
- options include aborting the repair, primary tissue repair, using a biologic mesh, or delayed repair
with synthetic mesh in 3 to 4 days
- the use of synthetic mesh in a grossly contaminated wound is contraindicated
- Risk Factors for Recurrence After Repair
- recurrence rates after incisional hernia repair may be as high as 30%
- hernia width and contamination are the 2 most significant risk factors for recurrence
- hernia length, hernia location (midline versus lateral), and significant comorbidities (e.g., obesity,
chronic obstructive pulmonary disease, diabetes, or smoking within 3 months of the operation) are
not as important for predicting recurrence
- Prevention of Incisional Hernias
- Laparotomy Closure Technique
- the technique and choice of suture material influences incisional hernia rates
- slowly (6–9 months) absorbable suture (polydioxanone, PDS) is preferred over rapidly (2–3 months)
absorbable suture (polyglactin, Vicryl)
- the rate of incisional hernias is lowest when small, closely spaced fascial bites are used
- 2 randomized trials using 2-0 polydioxanone and small, closely spaced fascial bites (5 mm deep
and 5 mm apart) demonstrated the lowest incisional hernia rate
- prophylactic onlay mesh reinforcement of elective midline laparotomy incisions reduces incisional
hernias but increases the rate of seromas and wound infections
- Parastomal Hernias
- Clinical Manifestations
- occurs in 50% of colostomies
- most are asymptomatic
- incarceration, bowel obstruction, or strangulation are rare
- routine repair is not recommended
- indications for repair include obstructive signs, difficulty applying an appliance, cosmesis
- Repair Techniques
- Primary Fascial Repair
- simplest option, but associated with the highest recurrence rate
- may be reinforced with mesh
- should only be used in patients who will not tolerate a laparotomy
- Stoma Relocation
- predisposes patient to another parastomal hernia in the future
- new stoma site may be reinforced with synthetic or biologic mesh
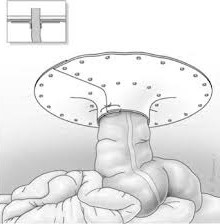
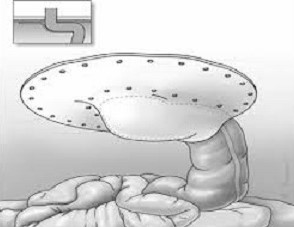
- Intraperitoneal Mesh Repair
- Keyhole Technique
- hernia is reduced and the defect closed primarily
- the site is then reinforced with a large piece of mesh which surrounds the ostomy
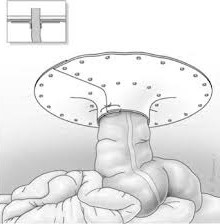
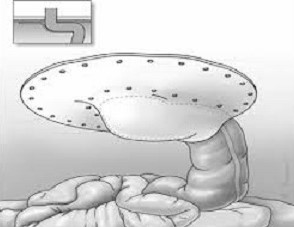
- Sugarbaker Procedure
- lateralizing the stoma redistributes the forces, minimizing hernia recurrence
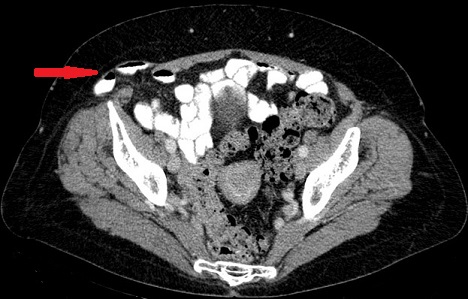
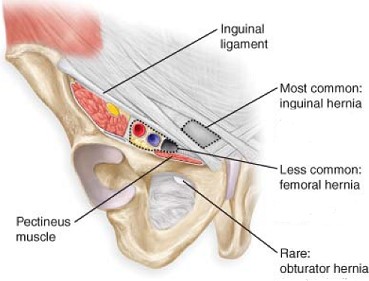
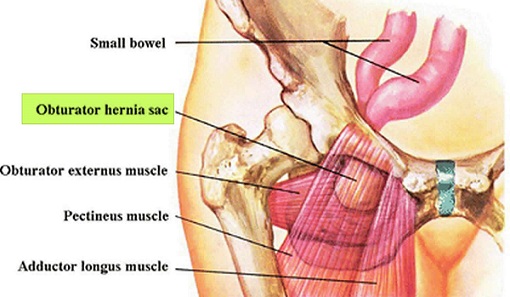
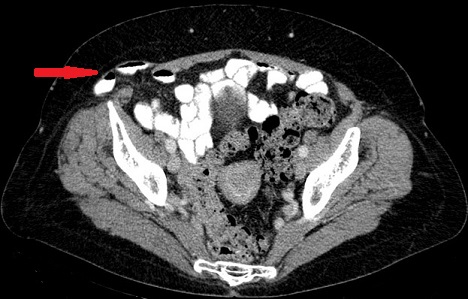
- Spigelian Hernias
- Anatomy
- defect in the semilunar line, usually below the arcuate line (where the posterior rectus fascia ends)
- may also result from surgical drains or laparoscopic ports
- hernia sac is usually below the external oblique fascia (interparietal)
- Clinical Presentation
- presents with localized pain but no bulge, because the hernia is below the intact external oblique fascia
- CT scan is usually required for the diagnosis
- should be repaired because of the high risk of incarceration
- Repair
- may be repaired open or laparoscopically
- in an open repair, the transversus abdominis and internal obliques muscles are repaired,
often without mesh
References
- Sabiston, 20th ed., pgs 1106 – 1116
- Cameron, 13th ed., pgs 631 - 635, 635 - 644, 650 - 656
- Schwartz, 10th ed., pgs 1449 - 1456
- SESAP 17. American College of Surgeons. Alimentary Tract.