Liver Abscesses and Hydatid Cysts
Pyogenic Abscesses
- Pathogenesis
- Biliary Tract Obstruction and Cholangitis
- most common mechanism
- after obstruction of the bile ducts, bacteria multiply and ascend into the intrahepatic biliary
radicals
- choledocholithiasis, benign and malignant strictures, and long-term palliative stents are the most
common etiologies
- Portal Vein Bacteremia
- formerly was the most common mechanism
- results from an intestinal infection such as appendicitis or diverticulitis
- Hepatic Artery Bacteremia
- results from systemic infections such as sepsis or endocarditis
- Direct Extension
- etiologies include gangrenous cholecystitis and subphrenic abscess
- Trauma
- bile leakage, hepatic necrosis, hematoma formation, and direct introduction of bacteria all
contribute to abscess formation after traumatic injury to the liver
- Necrosis of Hepatic Tumors
- associated with chemoembolization, alcohol injection, cryoablation or radiofrequency ablation of tumors
- Cryptogenic
- no cause is identified in ~ 20% of cases
- possible association with an occult colorectal cancer
- Pathology and Microbiology
- nearly equal distribution between solitary and multiple abscesses
- majority of abscesses are located in the right lobe only (60% - 75%), 20% are bilobar,
< 10% are in the left lobe only
- E. coli, Klebsiella, Staph Aureus, Streptococcus viridans, and Enterococcus are the most common aerobes isolated
- Bacteroides is the most common anaerobe isolated
- Candida is associated with immunosuppression, often from chemotherapy
- Clinical Manifestations
- Symptoms
- patients have a variable clinical presentation
- fever, chills, right upper quadrant pain are classic symptoms
- many patients will have only nonspecific symptoms: malaise, anorexia, nausea, vomiting, weight loss
- fever of unknown origin is also a common presentation
- Signs
- right upper quadrant tenderness, fever, hepatomegaly, and jaundice are possible physical findings
- Diagnosis
- Laboratory Studies
- leukocytosis is the most consistent lab abnormality
- elevated alkaline phosphatase and transaminases are nonspecific but frequent abnormalities
- elevated bilirubin implicates biliary obstruction as the etiology of the abscess
- blood cultures are positive in 40% - 50% of patients
- serologic testing will rule out an amebic abscess
- Imaging Studies
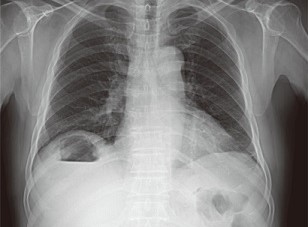
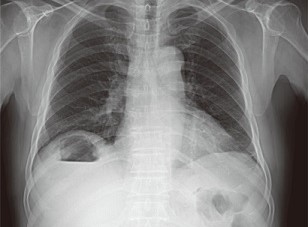
- Plain Films
- chest and abdominal x-rays may show nonspecific findings: right lower lobe atelectasis or
infiltrate, pleural effusion, elevated right hemidiaphragm
- occasionally a subdiaphragmatic air-fluid level may be seen
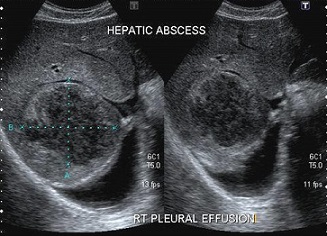
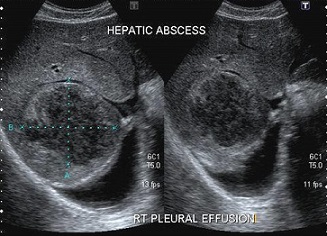
- Ultrasound
- useful screening test
- images the biliary tree more accurately than CT scan
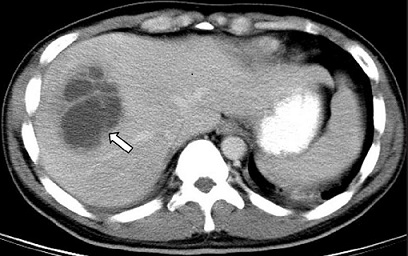
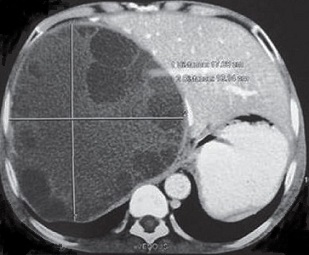
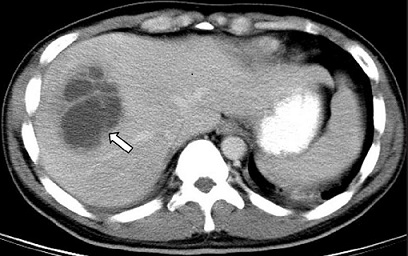
- CT Scan
- most sensitive and specific imaging procedure
- should be done with IV contrast, if possible
- peripheral rim enhancement or surrounding edema are specific for liver abscess
- may also reveal the underlying condition causing the abscess
- diagnostic or therapeutic procedures may be performed
- MRI
- as sensitive as CT for detecting liver abscesses
- in combination with MRCP, provides detailed information about the relationship of the abscess
with the biliary system
- Treatment
- most patients are treated with a combination of antibiotics and percutaneous drainage
- must also treat the underlying source
- Antibiotics
- empiric therapy should be started with IV antibiotics active against gram-negative rods,
streptococcus, and anaerobes
- antibiotic coverage is modified once culture results are ready
- IV therapy is given for 10 – 14 days, and oral antibiotics are continued for an additional month
- patients with multiple small abscesses not amenable to drainage may be treated with antibiotics alone
- Drainage
- Percutaneous Drainage
- mainstay of treatment, highly effective
- involves placement of an 8- to 14-French drainage catheter into the abscess cavity
under ultrasound or CT guidance
- may be used for both single and multiple abscesses
- care must be taken to avoid the pleural space
- aspiration without drain placement is often effective for abscesses < 5 cm in diameter
- Surgical Drainage
- most common indication is in patients who have an underlying condition requiring an operation
(appendicitis, diverticulitis, biliary disease)
- other indications include patients in whom percutaneous drainage is not advisable (coagulopathy,
ascites), multiple or multiloculated abscesses, or failure of percutaneous drainage
- most common approach is transabdominal; may also consider an anterior or posterior extraperitoneal
approach
- recently, laparoscopic drainage has been reported to have several advantages over percutaneous
drainage:
- the use of larger drainage catheters
- avoidance of transpleural drainage
- ability to search for and treat the underlying etiology
- Outcome
- pyogenic liver abscesses are 100% fatal without treatment
- with treatment, solitary abscesses have a 10% mortality and multiple abscesses a 40% mortality
Amebic Abscesses
- Epidemiology
- associated with tropical and subtropical environments and areas of poor sanitation
(India, Africa, Mexico, Central and South America)
- immigration from and travel to endemic areas make amebiasis a problem in the United States
(1% to 2% of the population)
- only 3% of 10% of patients with amebic infection will develop a liver abscess
- also associated with chronic immunosuppression (HIV, malnutrition, steroids)
- much higher incidence in males (10:1 ratio)
- Pathogenesis
- responsible pathogen is the protozoa Entamoeba histolytica
- this parasite exists in two forms, an immobile cyst and an invasive trophozoite
- humans are the principal host
- human infestation occurs by the fecal-oral route from ingesting cysts from contaminated
food or water or by direct contact
- the cystic form is ingested and is resistant to the acidity in the stomach
- the cyst wall is broken down by pancreatic enzymes in the small intestine, freeing the invasive trophozoite
- the trophozoite lives and multiplies in the large intestine
- in the majority of patients, no tissue invasion occurs
- when tissue invasion does occur, the trophozoites enter mesenteric venules and reach the liver
through the portal circulation
- if sufficient numbers of trophozoites accumulate in the liver, necrosis and liquefaction of hepatic
parenchyma occurs, giving rise to a single abscess cavity, usually in the right lobe
- antiamebic antibodies develop rapidly, but do not halt the progression of the disease
- the abscess cavity is sterile and odorless and composed of liquefied hepatic debris and blood (‘anchovy paste’)
- trophozoites are isolated only from the outer rim of the abscess cavity
- Diagnosis
- History
- patients will usually be males, age 20 – 40, who have recently travelled to or from an endemic area
- there may be an antecedent attack of intestinal amebiasis
- patients may present with an acute illness or a chronic indolent illness
- Symptoms
- right upper quadrant pain, fever and chills are the most common symptoms
- malaise, nausea, vomiting, anorexia, and weight loss also occur
- some patients may have pulmonary symptoms: cough, pleuritic pain, shortness of breath
- ~ 50% will have diarrhea
- Signs
- fever
- tender hepatomegaly is almost always present
- jaundice is rare
- Laboratory Studies
- diagnosis is made by an immunoassay which detects antibodies against the parasite
- stool studies for amoebas are positive in only a minority of patients
- leukocytosis and elevated liver function tests are common but nonspecific findings
- Imaging Studies
- ultrasound and CT scan are both appropriate studies
- lack of rim enhancement helps to distinguish between pyogenic and amebic abscesses
- aspiration is indicated primarily if the diagnosis between pyogenic and amebic abscess
is uncertain or if there is concern for a secondary bacterial infection

- Complications
- most dangerous complication is rupture into the pleural, peritoneal, or pericardial cavities
- secondary bacterial infection in 10% of cases
- Management
- Antibiotics
- most patients are successfully treated with amebicidal agents alone
- metronidazole is the most widely used agent and is successful in treating
both intestinal and extraintestinal amebiasis
- should begin empiric treatment while awaiting the result of serologic tests
- metronidazole should be given for 5 – 10 days, with a 95% success rate
- if the patient fails metronidazole, emetine or dehydroemetine may be tried
- intestinal colonization should be treated with a luminal agent such as iodoquinol
- Drainage
- percutaneous drainage is indicated in the following instances:
- diagnostic uncertainty
- concern for secondary infection
- persistent symptoms after 3 to 5 days of amebicidal therapy
- left lobe abscesses at risk for perforation into the pleural or pericardial spaces
Hydatid Cysts
- Epidemiology
- parasitic disease caused by the dog tapeworm, Echinococcus granulosis
- intermediate hosts include sheep and cattle; humans are an incidental intermediate host
- endemic areas include the Middle East, Iceland, Australia, New Zealand, southern Africa,
and the southern half of South America
- most reported cases in the United States have occurred in immigrants, especially from Greece and Italy
- Parasite Life Cycle
- tapeworm resides in the jejunum of dogs and produces eggs that are passed in the feces
- intermediate hosts then ingest the eggs by the fecal-oral route
- ingested eggs hatch in the gut of the intermediate host and the embryo passes through the mucosa
and enters the portal circulation
- most embryos lodge in the liver, but occasionally they may pass through the liver into the lungs
- once lodged in the liver, the cyst tends to grow progressively
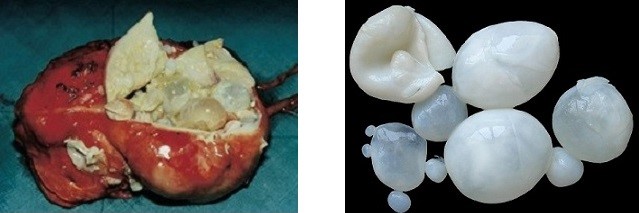
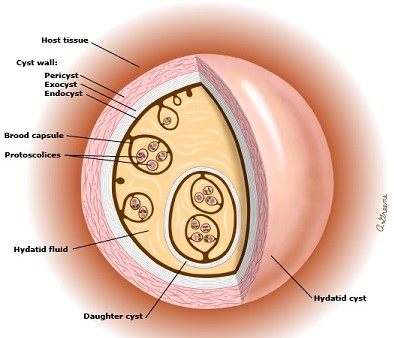
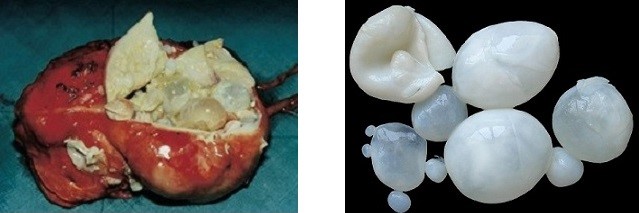
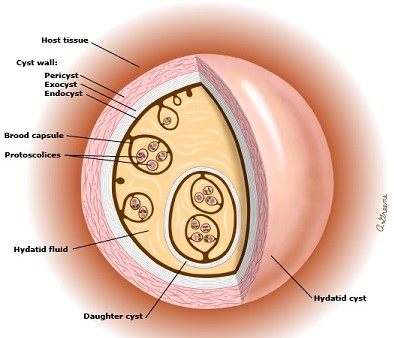
- Pathology
- 70% of hydatid cysts are located in the liver
- 75% are located in the right lobe
- grossly, the cyst has 2 layers: 1) the ectocyst, or pericyst, which is a fibrous adventitial layer contributed
by the host, 2) the parasite-derived endocyst, which has an outer laminated membrane and an
inner germinal layer
- the germinal layer generates brood capsules containing scolices and daughter cysts, which float freely
in the cyst fluid
- when brood capsules settle to the most dependent portion of the cyst, they are called hydatid sand
- a much less common form of the disease is caused by Echinococcus multilocularis, which causes an
invasive tumor-like replacement of liver tissue
- Complications
- intrabiliary rupture is the most common complication and occurs in 5% to 10% of cases
- abscess formation, the second most common complication, occurs secondary to contamination from bacteria
from the biliary tract
- intraperitoneal rupture may occur, leading to formation of new cysts in the peritoneal cavity and,
rarely, an anaphylactic reaction
- cysts may also grow craniad into the pleural cavity and rupture
- Clinical Manifestations
- most cysts are usually asymptomatic; many are found incidentally on routine imaging studies
- when they become symptomatic, the most common symptoms include right upper quadrant pain, tenderness,
and an abdominal mass
- with biliary rupture, the classic triad of biliary colic, jaundice, and urticaria may be seen
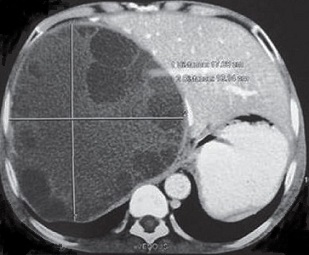
- Diagnosis
- diagnosis is made by a combination of clinical evaluation and imaging studies
- CT scanning is the imaging study of choice and will usually show a septated, calcified cystic mass with
daughter cysts and hydatid sand
- serologic tests may be performed in equivocal cases
- eosinophilia occurs in less than 25% of patients
- ERCP is an important study if rupture into the biliary tree has occurred
- Management of Uncomplicated Hydatid Cysts
- a small, densely calcified lesion can be assumed to be a dead hydatid and requires no therapy
- all live hydatids require treatment because of the likelihood of developing complications over time
- Surgery
- indications include biliary communication, cysts > 10 cm, multiple daughter cysts,
or percutaneous treatment is not available
- albendazole is usually started one week before surgery and continued for at least
four weeks postoperatively
- Simple Cystectomy
- involves removal of the cyst contents and lining wall and leaves only the patient’s
adventitial lining
- the cyst must be carefully packed off and isolated from the rest of the peritoneal cavity
to protect against spillage
- some surgeons inject scolicidal solutions (20% hypertonic saline) into the cyst prior to
removing the cyst contents
- bile leaks must be looked for and oversewn
- residual cyst cavity should be packed with omentum
- Pericystectomy
- entails dissection in the plane between the host adventitial layer
and the underlying liver tissue
- major operation associated with considerable blood loss
- does not have better results than simple cystectomy
- PAIR Procedure
- percutaneous procedure consisting of cyst puncture, aspiration of cyst contents,
injection of a scolicidal agent, reaspiration after 15 minutes
- done under US or CT guidance
- aim is to destroy the germinal layer with scolicidal agents
- contraindications include daughter cysts, biliary communication, and
superficial cysts at risk of rupture into the peritoneal cavity
- cure rate is > 95% in correctly chosen patients
- complications include cyst spillage into the abdominal cavity, biliary fistula,
chemical sclerosing cholangitis, bleeding and infection, local recurrence, and anaphylaxis
- albendazole should be given 4 hours before the procedure and for 1 month after
- Management of Complicated Hydatid Cysts
- Intrabiliary Rupture
- may cause biliary colic, obstructive jaundice, cholangitis, or pancreatitis
- cyst contents in the biliary tree can usually be managed by ERCP with sphincterotomy
- surgical common bile exploration may occasionally be required
- simple cystectomy is sufficient to manage the cyst
- the communication between the cyst and the bile duct must be carefully closed
- Intraperitoneal Rupture
- surgical emergency
- cyst is treated by simple cystectomy
- peritoneal cavity must be cleaned manually and by irrigation with 20% hypertonic saline
- long-term albendazole treatment is required (3 - 6 months)
- further surgery may be necessary if peritoneal cysts develop
References
- Schwartz, 10th ed., pgs 1284 - 1287
- Cameron, 11th ed., pgs 307-317, 341 - 346
- Sabiston, 20th ed., pgs 1445 – 1454
- UpToDate. Pyogenic Liver Abscess. Joshua Davis, PhD, MBBS, FRACP, Malcolm McDonald, PhD, FRACP, FRCPA.
Aug 17, 2018. Pgs 1 – 20
- UpToDate. Treatment of Echinococcosis. Pedro L. Moro, MD, MPH. Feb 20, 2020. Pgs 1 – 22