Evaluation
- History, Physical Exam, Lab Tests
- most benign tumors are clinically silent and are found incidentally on US or CT scan for other indications
- risk factors for hepatocellular carcinoma should be excluded: cirrhosis, chronic hepatitis
- must also exclude a prior extrahepatic malignancy
- symptoms to note include abdominal pain, weight loss, early satiety
- physical exam should detect signs of chronic liver disease, palpable liver mass, or other malignancy
- lab studies should check for anemia, liver function, and tumor markers (AFP, CEA, CA 19-9)
- Imaging
- cross-sectional imaging is the mainstay of diagnosis
- major tools are contrast-enhanced MRI and CT
- scans should be done with liver protocol: precontrast, early arterial phase, portal venous phase,
and equilibrium phase
- cystic versus solid is the first step in radiographic assessment
- solid lesions can be further characterized by their enhancement pattern on postcontrast imaging
- with contemporary imaging, the need for liver biopsy to establish a diagnosis is uncommon
Benign Lesions
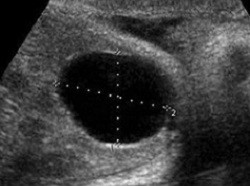
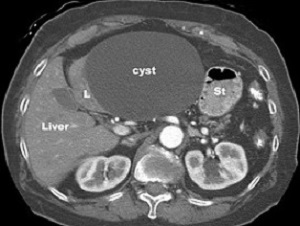
- Simple Cysts

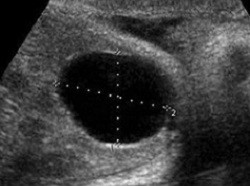
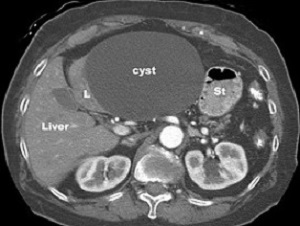
- simple cysts contain serous fluid, do not communicate with the biliary tree, and do not have septations
- complicated cysts suggest a biliary neoplasm: cystadenoma or cystadenocarcinoma
- occur in 5% of adults
- can be very large (up to 20 cm)
- usually are asymptomatic incidental findings on imaging
- if a patient is symptomatic, one must consider other sources for the symptoms before attributing
them to the cyst
- most common symptoms are from mass effect: early satiety from duodenal or gastric compression
- most common complication is intracystic hemorrhage, which rarely is life-threatening
- Management
- asymptomatic cysts do not require treatment or serial follow up
- needle aspiration should only be used to document a symptomatic response since the
cyst will always recur
- there is no evidence documenting long-term effectiveness of aspiration and sclerotherapy
- laparoscopic fenestration of the cyst is the treatment of choice, which involves excising the
cyst wall just above its margin with the liver

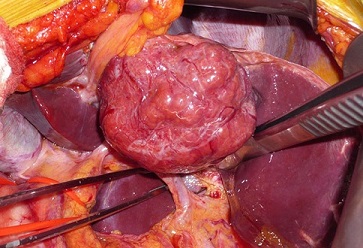
- Hemangioma
- most common benign neoplasm of the liver
- no risk of malignant degeneration
- very small risk of rupture or bleeding


- Clinical Manifestations
- most are incidentally found and are asymptomatic
- large lesions (> 10cm) can cause pain or mass effect symptoms
- giant cavernous hemangiomas can cause a DIC-type picture
- in the pediatric population, high-output cardiac failure from arteriovenous shunting can result
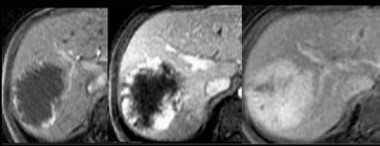
- Diagnosis
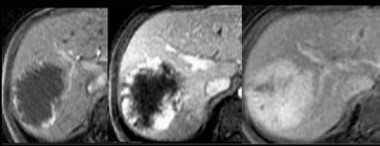
- multiphasic (liver protocol) CT or MRI is definitive
- typical characteristics include peripheral pooling of early phase contrast in the lesion,
followed by centripetal enhancement on later portal venous phase images
- biopsy is contraindicated because of the bleeding risk
- Management
- asymptomatic lesions can be observed, regardless of size
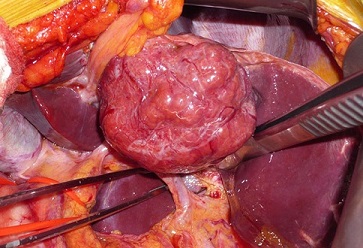
- for symptomatic lesions, enucleation is often technically possible
- anatomic resection may be necessary in some cases
- arterial embolization can be used preoperatively to shrink the lesion or as definitive
treatment in high-risk patients
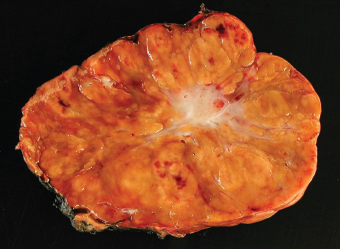
- Focal Nodular Hyperplasia
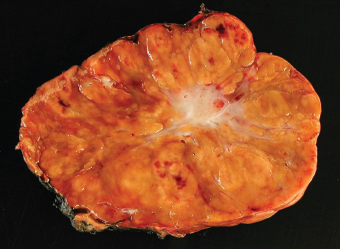
- Clinical Manifestations
- 2nd most common benign solid tumor of the liver
- may be a hyperplastic reaction to a congenital vascular malformation
- most common in young women (90%)
- oral contraceptives do not appear to be a risk factor
- no malignant potential
- do not rupture or bleed
- AFP is normal
- characterized by a central scar containing a large artery with multiple branches
radiating through the fibrous septa to the periphery of the lesion
- majority < 5 cm
- typically discovered incidentally on imaging or during laparoscopy
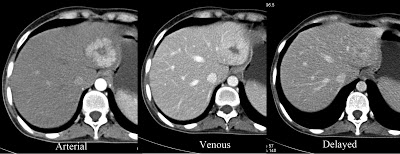
- Diagnosis
- FNH typically shows strong hypervascularity in the arterial phase of CT or MRI
with a central nonenhancing scar
- enhancement fades over time and becomes isointense to the liver parenchyma in the portal
and delayed phases
- on delayed imaging, the central scar may become hyperdense as contrast diffuses into the
fibrous center of the mass
- if no central scar is seen (15%), distinction between adenoma or fibrolamellar carcinoma
can be impossible
- since FNH contains Kupffer cells, radiolabeled sulfur colloid scans are positive in 60% of
FNH patients, and can be used in difficult to diagnose cases
- CT-guided biopsy usually reveals normal liver or suggests cirrhosis
- Management
- asymptomatic patients with typical imaging findings of FNH do not need resection
or long-term follow up
- no need to stop OCPs
- inability to rule out malignancy is the most common indication for surgery
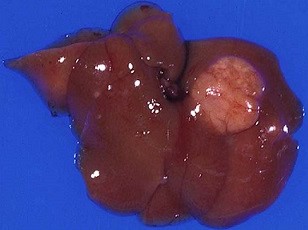
- Hepatic Adenoma
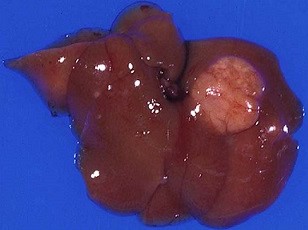
- Clinical Characteristics
- occurs most commonly in women between ages 20 – 40
- strong association with long-term OCP use
- anabolic steroid use is a risk factor for men
- familial adenosis polyposis and glycogen storage diseases are genetic syndromes associated with HCA
- major risks of HCA are rupture, necrosis, and malignant degeneration
- Symptoms
- most patients present with symptoms (50% - 75%)
- upper abdominal pain is common and may be related to hemorrhage into the tumor or
local compressive symptoms
- some patients may present acutely with rupture or intraperitoneal hemorrhage
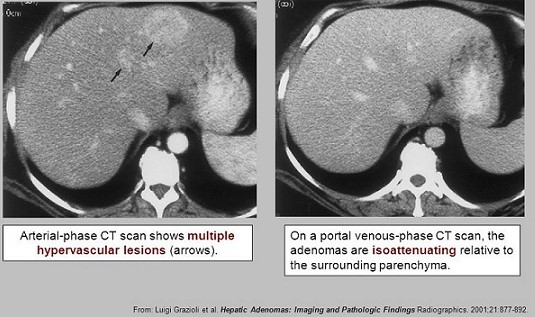
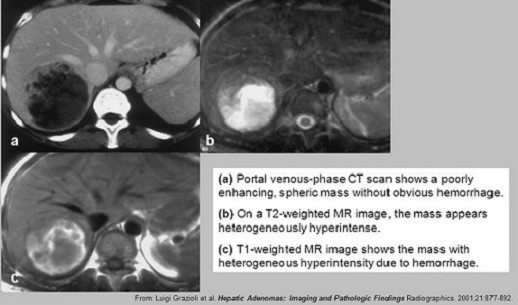
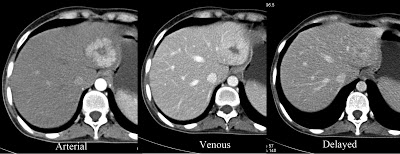
- Diagnosis
- AFP is normal unless there is malignant transformation
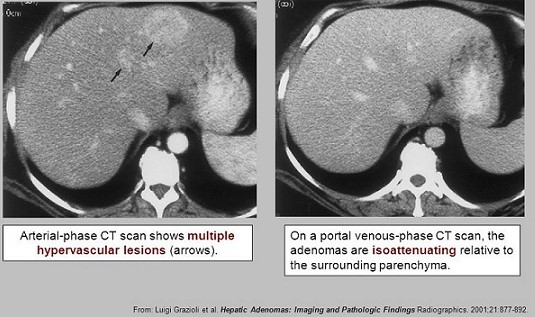
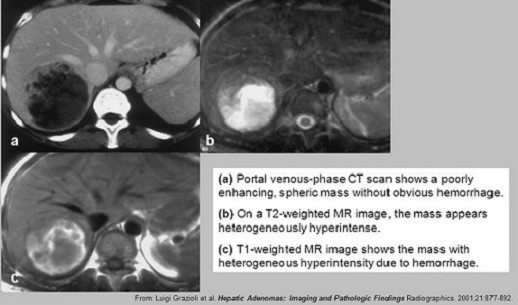
- on CT, adenomas have peripheral enhancement during the arterial phase,
centripetal progression during the portal phase, and become isodense during the late phase
- MRI typically reveals a well-demarcated heterogenous mass containing fat or hemorrhage
with arterial phase enhancement
- Classification
- HCAs can be subtyped based on their genotype
- the highest risk of malignancy is seen in adenomas with activating mutations in β-catenin
- preoperative biopsy and genetic analysis may become useful diagnostic and therapeutic tools in the future
- Management
- Intra-abdominal Hemorrhage
- embolization will usually control the acute hemorrhage, followed by elective resection
- if embolization is unsuccessful or unavailable, then an emergency operation is necessary,
and should be approached like a trauma laparotomy
- pringle maneuver, packing, selective hepatic arterial ligation are all possible
options for controlling bleeding
- resection should not be attempted in unstable patients
- in tumors ≥ 5 cm, risk of rupture is 30% - 50%
- Indications for Elective Resection
- symptomatic lesions
- inability to rule out malignancy
- size larger than 5 cm
- margin status is not important, and limited resections can be performed
- Asymptomatic Adenomas < 5 cm
- discontinue OCPs
- reimage with MRI in 6 months
- regression may occur after discontinuing OCPs
- resection is necessary if the lesion increases in size by 20% or becomes larger than 5 cm
- Pregnancy
- pregnancy is not contraindicated in women with adenomas < 5 cm
- since the behavior of adenomas during pregnancy is unpredictable,
some surgeons will recommend elective resection before pregnancy
- most surgeons will monitor the lesion with serial ultrasounds every 6 – 12 weeks during pregnancy,
and only recommend surgery if the lesion increases by more than 20% or becomes
larger than 5 cm
References
- Sabiston, 20th ed., pgs 1455 – 14585
- Cameron, 11th ed., pgs 322 - 327
- UpToDate. Approach to the Adult Patient with an Incidental Solid Liver Lesion.
Jonathan M Schwartz MD, Jonathan B Kruskal, MD, PhD. May 21, 2020. Pgs 1 – 29
- UpToDate. Hepatic Hemangioma. Michael P Curry, MD, Sanjiv Chopra, MD, MACP. Oct 28, 2019. Pgs 1 – 23
- UpToDate. Focal Nodular Hyperplasia. Sanjiv Chopra, MD, MACP. Nov 18, 2019. Pgs 1 – 18
- UpToDate. Hepatocellular Adenoma. Michael P Curry, MD, Nezam H Afdhal, MD, FRCPI. Apr 11, 2020. Pgs 1 – 25