Pancreas Anatomy and Physiology
Anatomy
- Embryology
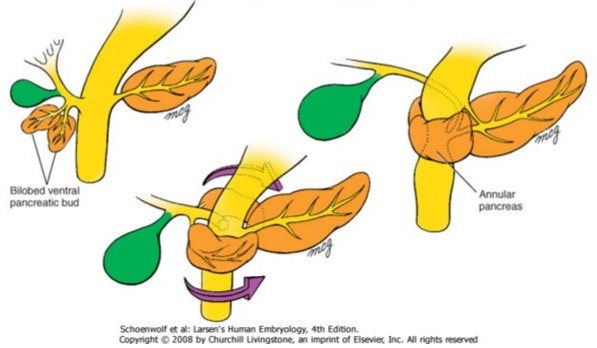
- the pancreas forms from 2 pouches, a larger dorsal pouch and a smaller ventral pouch
- the dorsal pouch forms first, directly from the duodenal endoderm, and forms the bulk of the
pancreatic tissue
- the ventral pouch develops as an outpouching from the hepatic diverticulum and maintains a close
relationship with the common bile duct
- as the duodenum rotates to assume its C configuration, the ventral pouch rotates clockwise
- at the 8th week of gestation, the ventral and dorsal pancreatic pouches fuse, as do their
respective duct systems
- the ventral pouch becomes the uncinate process and the inferior aspect of the pancreatic head
- the dorsal pouch becomes the superior aspect of the pancreatic head as well as the neck, body,
and tail of the gland
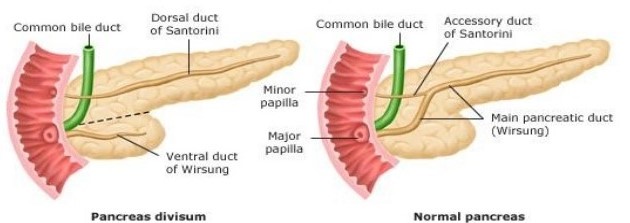
- the main pancreatic duct, the duct of Wirsung, joins the CBD in an intrapancreatic location and
empties through the ampulla of Vater at the major duodenal papilla
- the proximal aspect of the dorsal pancreatic duct, the duct of Santorini, may empty into the duodenum
through a separate minor papilla located ~ 2 cm above the major papilla
- Congenital Anomalies
- Heterotopic Pancreatic Tissue
- development of pancreatic tissue outside the confines of the main gland
- most commonly found in the stomach, duodenum, small intestine, and Meckel’s
diverticulum
- firm, yellow, irregular submucosal nodules that may vary from several millimeters
to several centimeters in size
- becomes clinically evident because of complications: intestinal obstruction,
usually as a result of intussusception, and ulceration and hemorrhage
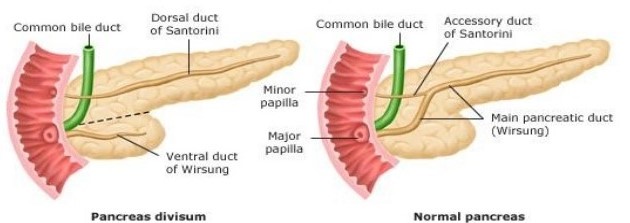
- Pancreas Divisum
- failure of fusion of the two primordial duct systems
- occurs in ~ 5% to 10% of the population
- major portion of the pancreas is drained by the duct of Santorini via the minor papilla
- a small duct of Wirsung drains through the major papilla
- the significance of pancreas divisum is controversial
- in some series of patients with idiopathic pancreatitis, the incidence of
pancreas divisum approaches 25%
- some have speculated that pancreas divisum, when associated with stenosis of the
minor papilla, may cause pancreatitis
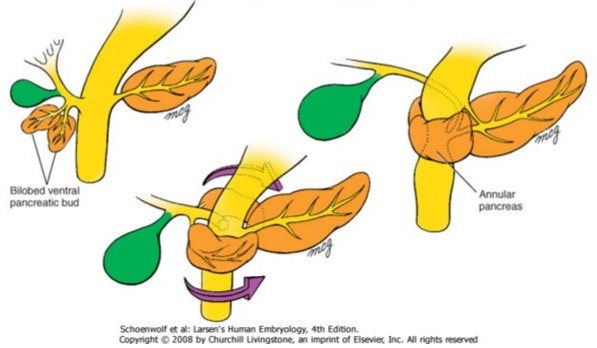
- Annular Pancreas
- histologically normal pancreatic tissue completely or partially encircles the
2nd portion of the duodenum
- thought to arise from failure of normal clockwise rotation of the ventral pouch
- often associated with other serious congenital anomalies
- obstructive symptoms are the indication for surgery
- a bypass – duodenojejunostomy or gastrojejunostomy – is the indicated procedure,
not resection or division of the obstruction
- Gross Anatomy
- the pancreas lies in the retroperitoneum, posterior to the stomach and lesser omentum
- covered by peritoneum anteriorly
- posteriorly the pancreas is in close proximity to the right renal vein, inferior vena cava, aorta,
superior mesenteric vein and artery, and splenic vein and artery
- divided into 5 portions: the head, uncinate process, neck, body, and tail
- the neck is anterior to the superior mesenteric vein
- the head is to the right of the neck and lies within the duodenal C loop
- the uncinate process arises from the inferior aspect of the head and extends posterior to the
superior mesenteric vein and ends at the right margin of the superior mesenteric artery
- the body is to the left of the neck
- the tail is to the left of the body and extends into the splenic hilum
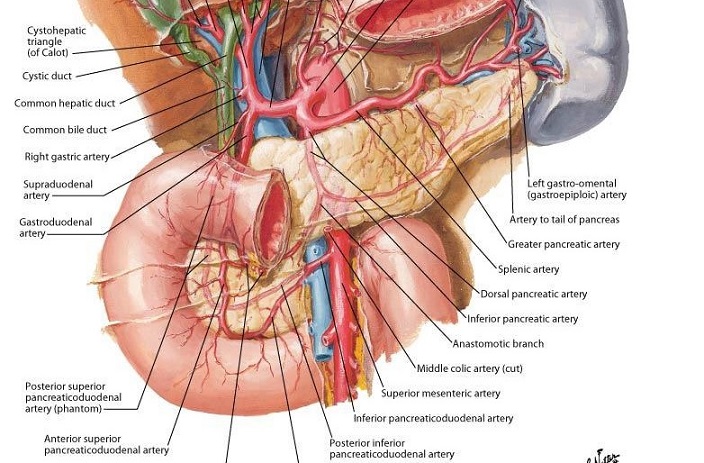
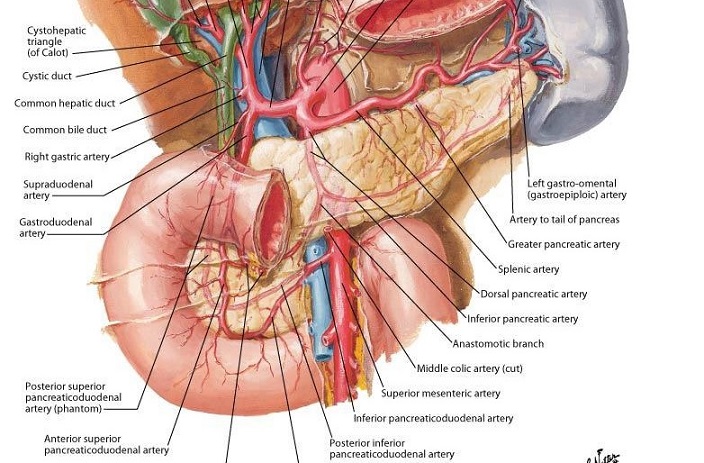
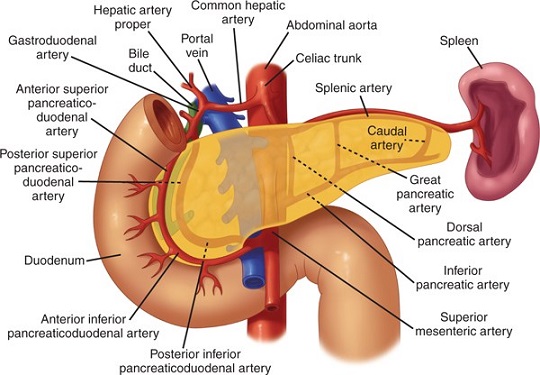
- Blood Supply
- Arterial Supply
- Head
- shares a joint blood supply with the 2nd portion of the duodenum
- supplied by a collateral network originating from the anterior and posterior
branches of the superior and inferior pancreaticoduodenal arteries
- the superior pancreaticoduodenal artery arises from the gastroduodenal
artery
- the inferior pancreaticoduodenal artery arises from the superior
mesenteric artery
- Neck, Body, and Tail
- generally supplied by a variable number of branches from the splenic artery
- within the posterior substance of the gland lies the inferior pancreatic artery,
which connects to the splenic artery via the transversely-oriented dorsal, great and caudal arteries
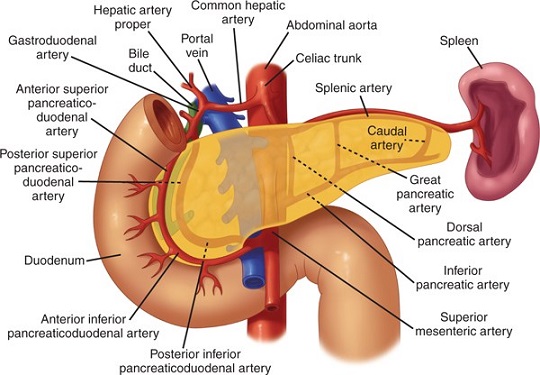
- Venous Drainage
- parallels the arterial anatomy
- eventually drains into the portal vein
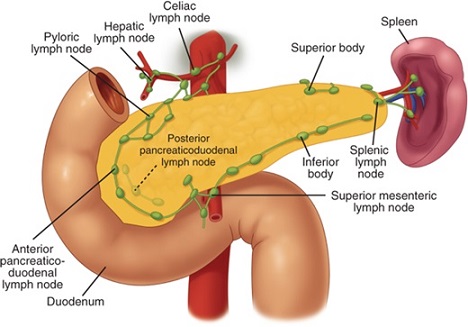
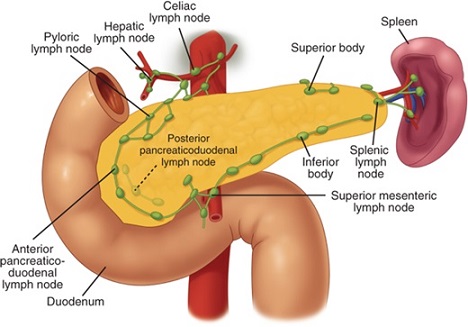
- Lymphatic Drainage
- extensive, with multiple lymph node groups draining the pancreas
- from the head of the gland, nodes in the pancreaticoduodenal groove drain into the
subpyloric, portal, mesocolic, mesenteric, and aortocaval nodes
- lymphatics in the body and tail drain into splenic nodes or into celiac, aortocaval,
mesocolic, or mesenteric nodes
- Innervation
- Sympathetic Innervation
- postganglionic sympathetic fibers, arising from the celiac ganglia, innervate the
pancreas and serve as the principal pathways for pain of pancreatic origin
- chemical splanchnicectomy is often performed for relief of pancreatic pain,
with variable success
- Parasympathetic Innervation
- originates from the posterior vagus nerve
- innervates the pancreatic islets, acini, and ducts
- Microscopic Anatomy
- 2 distinct organs reside within the pancreas, an exocrine organ and an endocrine organ
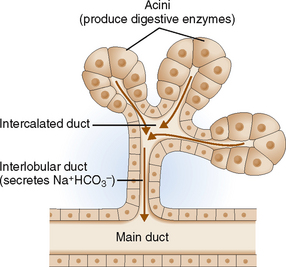
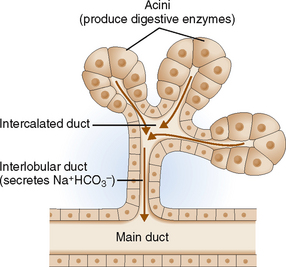
- Exocrine Pancreas
- comprised of the acini and ductal systems
- each acinus drains into a minor pancreatic duct
- the minor ducts terminate in the major pancreatic duct
- Endocrine Pancreas
- endocrine cells are contained within the islets of Langerhans
- the islets are spherical collections of cells scattered throughout the pancreas
- ~1,000,000 islets per gland
- each islet has an extensive blood supply and is composed of several different cell types
- each cell type produces a single hormone
- insulin-producing α cells are the most abundant (~70%), followed by
glucagon-producing β cells (20% to 25%)
- δ cells (5%) produce somatostatin, which appears to function as a paracrine modulator of islet cell function
- a small minority of islet cells produce pancreatic polypeptide (PP), vasoactive intestinal
peptide (VIP), and gastrin
Physiology
- Exocrine Pancreas
- Water and Electrolyte Secretion
- pancreas secretes 1 to 2 L/day of bicarbonate-rich fluid, which neutralizes
gastric acid in the duodenum and provides the optimal pH for the activity of
pancreatic enzymes
- under the control of the vagus nerve and the hormone secretin
- secretin, in turn, is released from the duodenum in response to luminal acid and is the
most potent stimulant of pancreatic bicarbonate secretion
- water and electrolyte secretion originates from the centroacinar and intercalated duct cells
- Digestive Enzyme Synthesis and Secretion
- synthesis and storage of over 20 different digestive enzymes occurs in the acinar cells
- enzyme secretion is stimulated by the vagus nerve and CCK
- CCK secretion is stimulated by the presence of protein and fat in the duodenum
- pancreatic enzymes are proteolytic (endopeptidases, exopeptidases), lipolytic
(lipase, colipase) and amylolytic (amylase)
- lipase and amylase are secreted in their active forms
- proteolytic enzymes are secreted in inactive forms
- proteolytic activation occurs after duodenal enterokinase cleaves trypsinogen to trypsin
- trypsin, in turn, activates the other proteolytic enzymes
- Endocrine Pancreas
- Insulin
- synthesized by the β cells in a precursor form, proinsulin
- primary stimulus for secretion is an increased blood glucose concentration
- performs many critical functions: 1) lowers blood glucose by enhancing cellular uptake,
2) stimulates glycogenesis, 3) inhibits gluconeogenesis, 4) stimulates lipogenesis,
5) inhibits lipolysis, 6) stimulates protein synthesis
- Glucagon
- synthesized by the α cells
- major stimulus for secretion is hypoglycemia
- counterbalances the effects of insulin and promotes hyperglycemia by causing hepatic
glycogenolysis and gluconeogenesis from proteins
- also relaxes and dilates smooth muscle such as the intestine and the sphincter of Oddi
- Somatostatin
- synthesized by δ cells
- acts in a paracrine as well as a classical endocrine fashion
- inhibits hormone release, gastric acid secretion, pancreatic exocrine secretion,
GI motor activity, and GI blood flow
- Pancreatic Polypeptide
- reported to decrease pancreatic exocrine secretion and bile secretion
- may also function as a glucoregulatory hormone
References
- Sabiston, 20th ed., pgs 1520 - 1524
- Schwartz, 10th ed., pgs 1341 - 1351
- Simmons and Steed, pgs 257 - 266