Small Intestine Anatomy and Physiology
Anatomy
- Gross Anatomy
- Duodenum
- lies in the retroperitoneum adjacent to the head and inferior border of the body of the pancreas
- separated from the stomach by the pylorus and from the jejunum by the ligament of Treitz
- arterial blood supply comes from both the celiac and superior mesenteric arteries
- Jejunum/Ileum
- the jejunum makes up the proximal two fifths of the small intestine, and the ileum makes up the
distal three fifths
- no distinct anatomic landmark separates the jejunum from the ileum; the ileum is separated from
the cecum by the ileocecal valve
- the jejunum has a larger diameter, thicker wall, and more prominent plicae circulares than the ileum;
the ileum has more abundant mesenteric fat
- suspended from the posterior abdominal wall by a broad-based mesentery that contains the blood supply
and lymphatics
- Blood Supply
- arterial supply is from the superior mesenteric artery
- vascular arcades in the mesentery provide an abundant collateral blood supply, although occlusion
of a major branch will lead to infarction of a segment of small bowel
- venous drainage parallels the arterial supply, ultimately draining into the superior mesenteric vein
- Lymphatics
- there is a rich lymphatic drainage of the entire small bowel
- there are 3 sets of mesenteric nodes: the first set is adjacent to the bowel wall, the second set is
adjacent to the mesenteric vascular arcades, the third set is along the trunk of the superior mesenteric artery
- from these nodes, lymph drains into the cisterna chyli and then the thoracic duct, eventually draining into the
venous system in the neck
- the lymphatics of the small intestine play a major role in lipid absorption and in immune defense
- Innervation
- has both sympathetic (splanchnic, inhibitory) and parasympathetic (vagus, excitatory) innervation
- in addition, the gut has an intrinsic neural network (enteric nervous system) that is able to function
independently from the extrinsic network
- Histology
- Mucosa
- contains an enormous absorptive surface area: the transverse folds (the plicae circulares),
the villi, the microvilli, and the glycocalyx covering the microvilli each greatly increase
the surface area exposed to luminal contents
- consists of 3 layers: the muscularis mucosae, the lamina propria, and the epithelium
- Epithelium
- the mucosal surface has two important structural features: the villi and the crypts of Lieberkühn
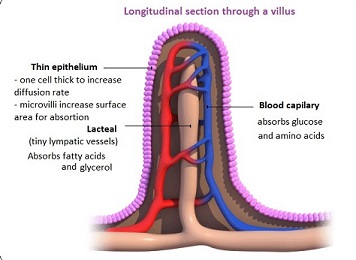
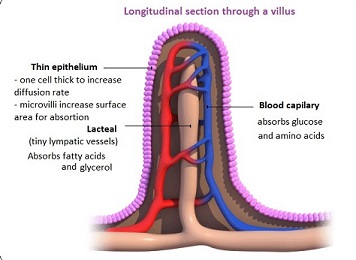
- Villi
- responsible for digestion and absorption
- covered by columnar epithelium
- each villus contains a lacteal, an artery, a vein, and a capillary network
- apical surface is covered by microvilli which contain the enzymes for the digestion of disaccharides and peptides
- Crypts
- contains 4 distinct cell types
- goblet cells secrete mucus
- endocrine cells secrete gastrin, secretin, cholecystokinin, somatostatin, enteroglucagon, motilin, neurotensin,
gastric inhibitory peptide
- Paneth cells secrete lysozyme and tumor necrosis factor and function in the host defense system
- undifferentiated cells replace lost absorptive cells (enterocytes)
- Submucosa
- layer of fibroelastic connective tissue containing collagen, blood vessels, nerves, and lymphatics
- strongest layer of the bowel
- Muscularis
- consists of 2 layers of smooth muscle: an outer longitudinal layer and an inner circular layer
- ganglion cells from the myenteric (Auerbach’s) plexus lie between the 2 muscle layers
- Serosa
- consists of visceral peritoneum
- encircles the entire jejunum and ileum
Physiology
- Digestion and Absorption
- Carbohydrate
- in a typical adult diet, 60% of carbohydrates are ingested as starch, 30% as sucrose,
and 10% as lactose
- Starch
- consists of 2 glucose polymers: amylose (20%) and amylopectin (80%)
- pancreatic and salivary amylase break down amylose and amylopectin into maltose (glucose-glucose),
maltotriose (glucose-glucose-glucose), and dextrins (the residual branched saccharides)
- these breakdown products are further broken down into glucose by enzymes located on the
microvilli brush border
- glucose, along with sodium, is then actively transported across the intestinal membrane by
carrier-mediated transport
- Sucrose
- disaccharide made up of glucose and fructose molecules
- broken down into individual glucose and fructose molecules by sucrase, an enzyme located on the
microvilli brush border
- Lactose
- disaccharide made up of glucose and galactose molecules
- broken down into glucose and galactose by lactase, which is located on the microvilli brush border
- Protein
- initial digestion begins in the stomach, where pepsin hydrolyzes proteins into polypeptides
- in the duodenum, pancreatic trypsinogen is activated to trypsin by the duodenal mucosal enzyme, enterokinase
- trypsin then activates the remaining pancreatic proteases
- the final products of protein digestion are amino acids and oligopeptides,
which enter the intestinal cell by sodium dependent, carrier-mediated active transport
- the oligopeptides are broken down into free amino acids by cytosolic peptidases
- digestion and absorption of proteins is 80% to 90% completed in the jejunum
- Fat
- fat in the duodenum stimulates the secretion of cholecystokinin and secretin,
resulting in gallbladder emptying and the secretion of pancreatic enzymes
- pancreatic lipase hydrolyzes triglycerides into 2 fatty acids and beta monoglyceride
- after this initial digestion, bile salts and lecithin combine with lipids to form micelles
- when the micelles encounter the brush border of the microvilli, the enclosed lipids diffuse
into the intestinal cell, a process which requires no energy
- once in the cell, the triglyceride is reformed in the smooth endoplasmic reticulum
- triglycerides then combine with cholesterol, phospholipids, and apoproteins to form chylomicrons
- chylomicrons preferentially enter the central lacteal of the villus, where they eventually enter the
thoracic duct and then the bloodstream
- normally, all ingested fat is absorbed
- jejunum is the site of most fat absorption
- Medium-Chain Fatty Acids
- C8 to C10 chain lengths
- may be absorbed without hydrolysis by lipase
- pass directly into portal blood without being formed into chylomicrons
- clinically, may be useful in the management of patients with deficiencies in fat digestion
and absorption
- Bile Salts
- the conjugated bile acids that form micelles are reabsorbed by active transport in the distal ileum
- reabsorbed bile acids then pass via portal venous blood to the liver, where they are resecreted in bile
(enterohepatic circulation)
- normal bile acid pool is about 5 gm and it recirculates six to eight times a day
- only 500 mg of bile acids are lost in the stool per day
- lost bile acids are replaced by hepatic synthesis from cholesterol
- Water, Electrolyte, and Mineral Absorption
- Water Absorption
- the small intestine secretes and absorbs huge amounts of water
- 1 to 2 liters of water per day are ingested
- in addition, salivary, gastric, biliary, pancreatic, and intestinal secretions contribute 5 to 10 liters
of water per day
- all but 500 cc of this fluid is reabsorbed in the small intestine
- osmotic pressure and diffusion are the forces governing movement of water across the intestinal cell membrane
- osmotic pressure results from the active transport of solutes (sodium, glucose, amino acids) into the intestinal cell
- diffusion occurs through pores in cell membranes
- Electrolyte Absorption
- in the jejunum, sodium is usually cotransported along with glucose and amino acids
- in the ileum, sodium is absorbed against a steep electrochemical gradient
- potassium is passively absorbed along its electrochemical gradient
- chloride is absorbed by active transport and by coupling to organic solutes
- bicarbonate is absorbed by active transport
- Mineral Absorption
- calcium is absorbed in the duodenum and proximal jejunum by active transport and is
facilitated by an acid environment, vitamin D, and parathyroid hormone
- iron is absorbed in the duodenum
- magnesium absorption occurs in the ileum, predominantly by passive diffusion
- Vitamin Absorption
- fat-soluble vitamins first become incorporated into micelles, and then pass freely into intestinal cells where they
packaged into chylomicrons before entering the lymphatic system
- ileum is the major site of vitamin C absorption
- vitamin B12 absorption occurs in the distal ileum and requires binding to gastric intrinsic factor
- Motility
- Migrating Myoelectric Complex (MMC)
- between meals, there are cyclically occurring contractions that move down the intestine every 90 minutes
- most of these contractions originate in the stomach or duodenum
- the purpose may be to sweep the intestine clean between meals
- motilin appears to regulate the MMC
- Regulation of Motility
- pacesetter potentials, probably originating in the duodenum, initiate contractions that propel
food through the small intestine
- 2 types of contractions: segmentation and peristalsis
- sympathetic activity inhibits intestinal motility; parasympathetic activity increases it
- denervation of the small intestine does not produce long-term disturbance of function
- many hormones influence intestinal motility: gastrin, cholecystokinin, and motilin stimulate
muscle contraction; secretin, glucagon, and somatostatin inhibit muscle contraction
- Endocrine Function
- Secretin
- primarily found in duodenal S cells
- released in response to intraluminal acid
- stimulates the release of water and bicarbonate from the pancreas, neutralizing gastric acid
- also inhibits gastrin release, gastric acid secretion, and gastrointestinal motility
- Cholecystokinin
- release is stimulated by amino acids and fatty acids
- causes gallbladder emptying and relaxation of the sphincter of Oddi
- stimulates the secretion of pancreatic enzymes
- Other Gut Hormones
- Enteroglucagon
- found primarily in the distal small intestine
- major action is to inhibit intestinal motility
- Vasoactive Intestinal Peptide
- functions chiefly as a neuropeptide
- potent vasodilator
- stimulates pancreatic and intestinal secretions
- inhibits gastric acid secretion
- is the primary agent in the watery diarrhea syndrome caused by pancreatic
endocrine tumors (VIPomas)
- Motilin
- Somatostatin
- paracrine agent
- functions as an ‘off’ switch to inhibit GI hormone release
- Immune Function
- the large surface area of the small bowel mucosa represents a huge potential portal of entry for pathogens
- the small bowel is a major source of immunoglobulin A, which is produced by plasma cells located in the lamina propria
- IgA antibody binds to a carrier protein and is secreted into the intestinal lumen
- the antibodies collect in the glycocalyx, where they are best able to interact with antigen
- antigens from the intestinal lumen are transported through specialized epithelial cells called M cells that are in contact
with underlying lymphoid cells
- antigens then come into contact with macrophages, leading to the secretion of interleukin-1 and activation of helper T cells
References
- Schwartz, 10th ed., pgs 1137 - 1145
- Sabiston, 20th ed., pgs 1237 - 1247
- Simmons and Steed, pgs 234-241