Postgastrectomy Syndromes
Anastomotic Complications
- Afferent Limb Obstruction
- Clinical Manifestations
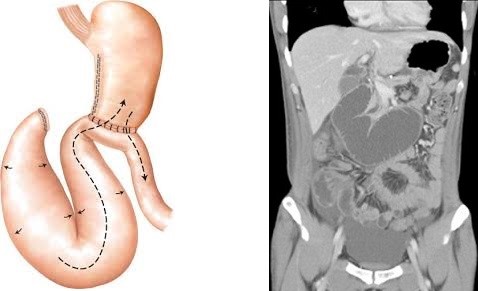
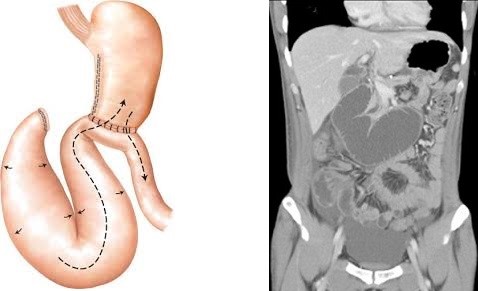
- occurs only after a Billroth II reconstruction (gastrojejunostomy)
- caused by intermittent obstruction of the afferent limb, with accumulation of biliary and pancreatic secretions
- intraluminal pressure gradually increases, eventually causing the afferent limb contents to decompress into the stomach
- main symptom is colicky epigastric or right upper quadrant pain relieved by bilious vomiting
- Diagnosis
- CT scan may show a dilated afferent limb
- endoscopy may not visualize the afferent limb
- barium upper GI may also demonstrate a dilated afferent limb
- biliary radionuclide scans (HIDA) will also show a dilated afferent limb
- Treatment
- always surgical
- main technical problem is a long afferent limb
- in the early post op period, immediate operation is required to prevent a duodenal stump blowout
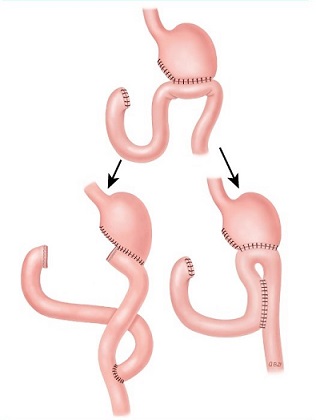
- standard approaches are a revision of the gastrojejunostomy or a conversion of the gastrojejunostomy to a Roux-en-Y
- another approach is to decompress the afferent limb with a side to side anastomosis to a proximal segment of jejunum
(Braun enteroenterostomy)
- Efferent Limb Obstruction
- Clinical Manifestations
- mechanical obstruction causing epigastric pain, distention, and bilious vomiting
- must be distinguished from afferent limb syndrome or alkaline reflux gastritis
- usually diagnosed by a CT scan or UGI that shows failure of the contrast to enter the efferent limb
- Treatment
- surgical correction is directed towards the underlying etiology (adhesions, internal herniation)
- may require the creation of a new anastomosis
- Duodenal Stump Leak (Blowout)
- most commonly occurs 7 – 10 days after a BII gastrojejunostomy, and is often associated with an afferent
limb obstruction
- patients may present with fever, tachycardia, hypotension, and/or peritonitis
- CT scan is the diagnostic test of choice
- surgery is required for wide drainage and insertion of a duodenostomy tube
Motility Complications
- Dumping Syndrome
- Early Dumping Syndrome
- Symptoms
- most commonly occurs after a partial gastrectomy with Billroth II reconstruction
- symptoms occur 20 – 30 minutes after a meal
- GI symptoms predominate: nausea/vomiting, epigastric fullness, cramping abdominal pain,
often explosive diarrhea
- cardiovascular symptoms include palpitations, tachycardia, diaphoresis, dizziness, flushing, fainting
- a high carbohydrate meal usually precipitates the attack, but it can occur after any meal
- Pathophysiology
- destruction of the pylorus allows rapid emptying of hyperosmolar chyme, especially carbohydrates,
into the intestine
- the net effect is rapid fluid shifts into the small intestine to achieve isotonicity
- this results in the release of vasoactive hormones such as serotonin and vasoactive intestinal peptide (VIP)
- gastric emptying studies often document rapid liquid emptying
- underlying cause may be related to the loss of receptive relaxation: gastric pressure increases during a meal
and then decompresses through the gastric outlet procedure
- Treatment
- Medical
- great majority of cases resolve spontaneously
- some patients respond to eating frequent small meals low in carbohydrates
- separating solids and liquids at meals can help
- in refractory cases, the administration of octreotide, a somatostatin analog, is often beneficial
- Surgery
- only used if dietary manipulations and octreotide fail to control the symptoms
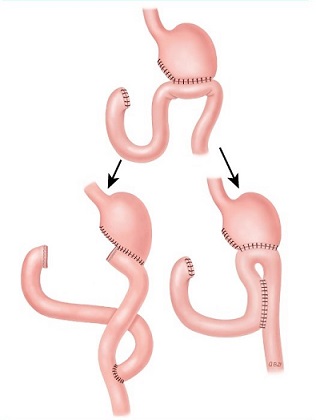
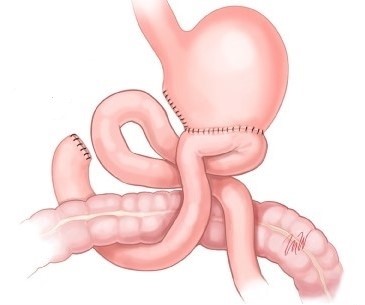
- the operation of choice is conversion of the gastrojejunostomy to a Roux-en-Y
- a 45 - 60 cm Roux limb is constructed and placed in an antecolic fashion
- the gastric remnant should be less than 25% to avoid Roux stasis syndrome
- Late Dumping Syndrome
- Symptoms
- similar symptoms as early dumping, but occurs 1 to 2 hours after a meal
- related to hypoglycemia
- Pathophysiology
- rapid emptying of carbohydrates into the intestine causes postprandial hyperglycemia
- hyperosmolar material in the intestine results in the release of enteroglucagon
- enteroglucagon sensitizes the pancreatic islets to release excessive amounts of insulin,
resulting in an ‘overshoot’ hypoglycemia
- hypoglycemia results in catecholamine secretion
- Treatment
- similar to that for early dumping
- patients should be placed on a low carbohydrate diet
- revisional surgery is almost never required
- Postvagotomy Diarrhea
- Clinical Manifestations
- diarrhea occurs is up to 30% of patients following truncal vagotomy
- most patients have mild symptoms; only 1% to 2% of patients have incapacitating symptoms
- Pathogenesis
- etiology is unclear
- may be related to rapid transit of bile acids from the denervated biliary tree into the colon
- Treatment
- Medical
- dietary alterations can be helpful: smaller and more frequent meals and more dietary fiber
- cholestyramine has been used to bind bile salts
- antidiarrheal agents are used to reduce the number of stools
- octreotide has also been used with good results
- Surgery
- used only as a last resort
- the goal of surgery is to slow intestinal transit
- a 10 cm antiperistaltic jejunal segment interposed 100 cm distal to the ligament of Treitz has been
used with some success, but it may cause obstructive symptoms or bacterial overgrowth
- Acute Gastroparesis
- Clinical Manifestations
- incidence varies from 10% to 50% following gastric operations, especially if a truncal vagotomy was
part of the procedure
- also seen after a Whipple resection and palliative gastrojejunostomy
- symptoms include persistently high nasogastric tube outputs or vomiting following oral intake
- Treatment
- Medical Therapy
- need to rule out mechanical obstruction with a barium study or endoscopy
- if the anastomosis is patent, then a period of nasogastric decompression,
hyperalimentation, and administration of prokinetic agents is begun
- Reglan, Cisapride, and erythromycin may all be tried
- a percutaneous gastrostomy tube may be inserted so that the nasogastric tube can be removed
- most cases will resolve within 3 to 4 weeks
- Surgery
- surgery is reserved for the most refractory cases
- surgical goal is to remove a portion of the atonic stomach by a further gastric resection
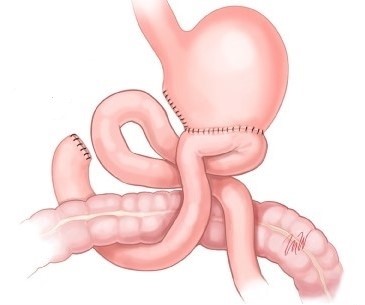
- if the remaining stomach is > 25%, then reconstruction should be with a BII; if it is < 25%,
then a Roux-en-Y will be necessary
- if a BII reconstruction is performed, then a distal Braun enteroenterostomy should be done to
divert bile away from the stomach, eliminating postoperative bile reflux
- Chronic Gastroparesis
- Clinical Manifestations
- characterized by nausea, ± vomiting, abdominal pain, bloating, frequent bezoar formation
- endoscopy and barium studies are necessary to rule out an anastomotic stricture
- Treatment
- Medical Therapy
- prokinetic agents are usually empirically started
- the efficacy of these agents can be evaluated by radionuclide gastric emptying studies
- Surgery
- goal of surgery is to remove a portion of the atonic stomach
- if the patient has had a vagotomy/pyloroplasty, then a hemigastrectomy is performed
- if the patient has had a prior antrectomy or hemigastrectomy, then an additional resection
is performed
- Bile Reflux Gastritis
- Clinical Manifestations
- symptoms include severe upper abdominal burning pain that worsens after a meal, chronic nausea,
and bilious vomiting
- Diagnosis
- diagnosis is primarily one of exclusion
- differential diagnosis includes marginal ulceration, afferent loop syndrome, anastomotic stricture,
and chronic gastroparesis
- a barium study can be used to rule out an anastomotic stricture and afferent loop syndrome
- endoscopy will show marked gastritis that should be confirmed by biopsy
- gastric emptying studies should be performed to rule out chronic gastroparesis
- HIDA scan can demonstrate bile reflux into the stomach
- Treatment
- Medical Therapy
- no specific medical treatment has proven effective
- Carafate has been used to ‘coat and protect’ the stomach
- Surgery
- 45 - 60 cm Roux-en-Y adequately diverts the bile away from the stomach
- must be certain that the patient does not have gastroparesis, since a Roux-en-Y diversion
will only exacerbate this problem
- in patients with gastroparesis, an enteroenterostomy between the afferent and efferent limbs
of the gastrojejunostomy should be sufficient
- The Roux Stasis Syndrome
- Clinical Manifestations
- severe gastroparesis following a Roux-en-Y gastrojejunostomy
- the early syndrome resolves with time and prokinetic agents, especially erythromycin
- the chronic syndrome presents with abdominal pain, vomiting, and often bezoar formation
- Diagnosis
- endoscopy is usually normal
- barium studies may show a dilated Roux limb with no evidence of distal obstruction
- gastric emptying studies will show delayed gastric emptying
- GI motility studies show disordered motility in the Roux limb, with propulsive activity towards
the stomach, rather than away
- Treatment
- Medical Therapy
- erythromycin is useful in the short-term, but it is less useful chronically
- Surgery
- standard surgical approach is to convert the patient to a subtotal or near-total gastrectomy,
recreating a new Roux-en-Y reconstruction
- another approach is to perform a subtotal gastrectomy, take down the Roux limb, and perform a
Billroth II reconstruction with a distal Braun enteroenterostomy
- the goal of this second procedure is to restore gastric emptying, but at the same time maintain
adequate biliary diversion
Long-Term Complications
- Peptic Ulcers
- may occur in the stomach, duodenum, or jejunum (marginal ulcers)
- incomplete vagotomy is now a rare reason for ulceration in postgastrectomy patients
- the most common cause today is retained gastric antrum
- Retained Gastric Antrum
- antral tissue may be left on the duodenal margin of resection
- this retained antral tissue secretes high levels of gastrin since it is not inhibited by gastric acid
- the resulting hypergastrinemia causes excessive gastric acid secretion, resulting in ulceration
- the diagnosis is made by an elevated fasting gastrin level that is suppressed by IV secretin – gastrinoma patients
have a paradoxical increase in gastrin with secretin administration
- the treatment for retained antrum is surgical resection of the remaining antrum and first portion of the duodenum
- Gastric Remnant Cancer
- patients who have had a partial gastrectomy for benign disease are at an increased risk for developing gastric cancer
- these cancers typically occur 15 – 20 years after the initial surgery
- most often occur near the gastrojejunal anastomosis
- the etiology is thought to be chronic inflammation from reflux of bile and pancreatic secretions
Metabolic Complications
- Anemia
- most common metabolic problem in postgastrectomy patients
- iron absorption in the proximal intestine is facilitated by an acidic environment
- vitamin B12 and folate deficiency also contribute to anemia
- Weight Loss
- altered dietary intake is multifactorial: small residual reservoir, gastroparesis, anorexia secondary to ghrelin loss,
food restriction because of diarrhea or dumping
- fat malabsorption can occur because pancreatic lipase is activated by acid
- Bone Disease
- osteoporosis and osteomalacia are caused by calcium and vitamin D deficiency
- calcium absorption occurs primarily in the duodenum, which is bypassed with a gastrojejunostomy
- fat-soluble vitamins (A, D, E, K) may be poorly absorbed because of inadequate mixing of pancreatic enzymes and food
- Gallstones
- results from vagal denervation of the gallbladder, leading to gallbladder dysmotility and stasis
- should consider cholecystectomy at the time of gastric surgery if the patient has gallstones
References
- Schwartz, 10th ed., pgs 1090 - 1095
- Sabiston 20th ed., pgs 1212 - 1213
- Cameron 7th ed., pgs 90-100
- UpToDate. Postgastrectomy Complications. Ashley MD, Stanley. Apr 12, 2019. Pgs 1 – 29