Thyroid Anatomy and Physiology
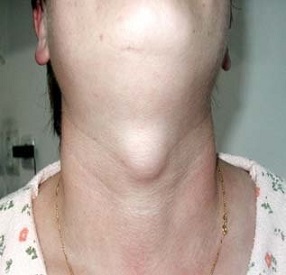
Thyroid Anatomy
- Embryology
- thyroid originates from the base of the tongue (foramen cecum)
- descends along the thyroglossal tract anterior to the hyoid bone and larynx
- descending thyroid is joined laterally by parafollicular cells from the neural crest -
these cells secrete calcitonin
- Lingual Thyroid
- thyroid develops but fails to descend
- usually presents as a posterior tongue mass
- may represent the patient’s only functioning thyroid tissue
- diagnosis made by thyroid scan
- treatment consists of thyroid suppression with thyroxine
- malignancy is rare
- Thyroglossal Duct Cyst
- arises from persistence of a portion of the thyroglossal tract (duct)
- usually presents as a midline neck mass in childhood or adolescence
- diagnosis can be made by asking the patient to protrude his tongue - a thyroglossal
cyst should move upward
- treatment is surgical excision and should include the entire thyroglossal duct remnant
as well as the central portion of the hyoid bone (Sistrunk procedure)
- ~ 1% of thyroglossal duct cysts contain thyroid cancer
- Lateral Aberrant Thyroid
- now felt to represent a well-differentiated thyroid cancer that has metastasized to a
cervical lymph node
- the primary tumor is usually found in the ipsilateral thyroid lobe
- Surgical Anatomy
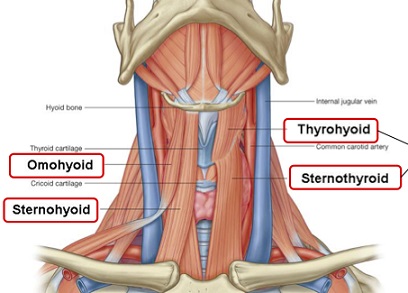
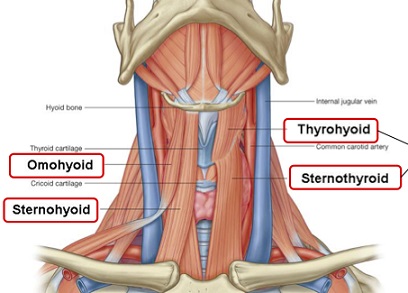
- Strap Muscles
- cover the thyroid anteriorly
- innervated by the ansa cervicalis
- sternothyroid muscle lies deep to the sternohyoid muscle
- Blood Supply and Lymphatic Drainage
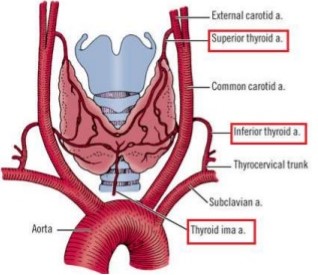
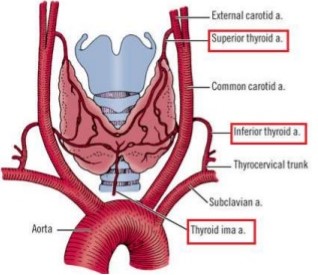
- Arterial Supply
- paired superior thyroid arteries arising as the first branch of the external carotid
- paired inferior thyroid arteries arising from the thyrocervical trunk of the subclavian arteries
- occasionally the thyroid ima is present, arising from the aortic arch or innominate artery
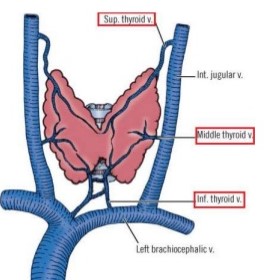
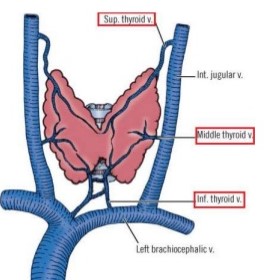
- Venous Drainage
- superior thyroid veins → internal jugular vein
- middle thyroid veins → internal jugular vein
- inferior thyroid veins → brachiocephalic vein
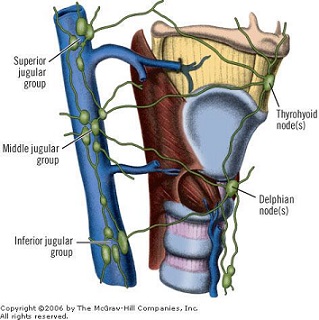
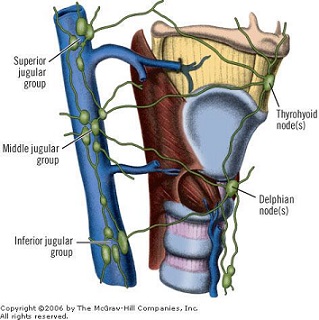
- Lymphatic Drainage
- categorized according to superior, inferior, and lateral drainage patterns
- superior aspect of the isthmus and median aspects of the lateral lobes drain upward
into the prelaryngeal (delphian) nodes
- inferior lymph vessels follow the inferior thyroid veins to drain into the pretracheal
and innominate nodes
- lateral lobes drain into the internal jugular nodes
- Parathyroid Glands
- usually closely related to the thyroid and are covered by the thyroid sheath
- upper glands are more posterior, and may descend into the posterior mediastinum
- lower glands are more variable in position but are usually anterior to the recurrent laryngeal nerves,
and may descent into the thyrothymic tract or thymus gland
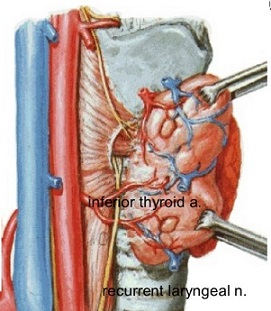
- blood supply of all glands comes from the inferior thyroid artery
- Laryngeal Nerves
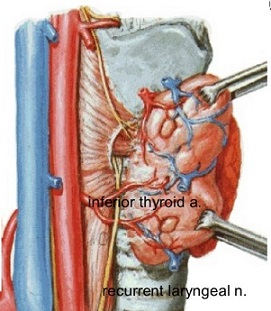
- Recurrent Laryngeal Nerve
- branch of the vagus nerve
- innervates all the muscles of the larynx except the cricothyroid
- unilateral injury leads to vocal cord paralysis and hoarseness, as well as ineffective cough
and aspiration
- bilateral injury leads to complete loss of voice and airway obstruction
- on the right, the recurrent nerve loops under the subclavian artery
- on the left, the recurrent nerve arises at the level of the aortic arch and loops
beneath the ligamentum arteriosum
- usually ascends upwards in the tracheoesophageal groove
- may run behind the inferior thyroid artery, between its branches, or in front of it
- in ~ 1% of cases, the right nerve is nonrecurrent and enters the larynx directly
- Superior Laryngeal Nerve
- also arises from the vagus nerve
- at the level of the hyoid bone, it splits into internal (sensory) and external (motor) branches
- external branch travels with the superior thyroid artery and innervates the cricothyroid muscle
- cricothyroid muscle alters vocal cord tension and affects the pitch of the voice
- injury to the superior laryngeal nerve results in a loss of timbre and volume in the voice,
making singing and shouting difficult
- to avoid injury, the superior pole thyroid vessels should be ligated and divided low on the thyroid gland
Thyroid Physiology
- Thyroid Follicle
- functional unit of the thyroid gland
- sphere of cuboidal epithelium containing a central core of colloid
- contains a rich capillary network
- Iodine Metabolism
- formation of thyroid hormone is dependent on the availability of exogenous iodine
- average daily iodine requirement is 0.1 mg and is found mainly in fish, milk, and eggs
- in the U.S., iodine is routinely added to bread and salt
- iodine is rapidly reduced to iodide in the stomach and jejunum
- under the influence of thyroid stimulating hormone (TSH), iodide is actively transported into
the thyroid follicular cells
- Synthesis of Thyroid Hormone
- inside the follicular cell, iodide diffuses through the cytoplasm to the apical membrane,
where it is oxidized by peroxidase back to iodine
- iodine then binds to tyrosine residues on the thyroglobulin molecule to form monoiodotyrosine
(MIT) and diiodotyrosine (DIT)
- 2 molecules of DIT combine to form thyroxine (T4); MIT and DIT combine to form T3 or reverse T3 (rT3)
- coupling steps are catalyzed by peroxidase
- TSH positively regulates the iodination and coupling process
- antithyroid drugs (propylthiouracil, methimazole) are competitive inhibitors of peroxidase
- in high doses, iodide blocks iodide uptake by the thyroid as well as hormone synthesis
- Storage and Secretion of Thyroid Hormone
- T4 and T3 are bound to thyroglobulin and stored in the colloid of the thyroid follicles
- thyroglobulin is a glycoprotein that is virtually the sole constituent of follicular colloid
- in response to TSH, the follicular cell reabsorbs thyroglobulin by endocytosis
- thyroglobulin then fuses with lysosomes containing hydroxylases
- hydrolysis results in release of T4, T3, rT3, MIT, and DIT
- MIT and DIT undergo deiodinatination in the thyroid cell and the iodide is reused in the cell
- T4, T3, and rT3 are released into the circulation
- Metabolism of Thyroid Hormone
- T4 is the major thyroid hormone released
- 80% of circulating T4 undergoes peripheral conversion in the kidney and liver to T3 and rT3
- T3 is 10 times as biologically active as T4
- rT3 is biologically inactive
- 99.98% of thyroid hormone is reversibly bound to 3 plasma proteins: thyroid-binding globulin (TBG),
thyroid-binding prealbumin (TBPA), and albumin
- TBG may be increased as a result of the estrogen effects of pregnancy or oral contraceptives
- increased TBG results in a higher circulating amount of T4 because of increased serum binding capacity,
but the active free T4 levels remain unchanged
- Molecular Basis of Thyroid Hormone Action
- unbound thyroid hormones are transported across cell membranes by diffusion
- at the cellular level, T3 is the active hormone
- T3 binds to specific receptors located in the cell nucleus
- T3/T3 receptor complex then binds to regulatory regions of genes and modifies their transcription
- Regulation of Thyroid Activity
- TSH
- principal agent that modulates thyroid function and thyroid cell growth
- produced by the anterior pituitary
- stimulates iodide uptake, iodination of thyroglobulin, and promotes release of T3 and T4
from thyroglobulin
- stimulates gene transcription and synthesis of thyroglobulin and thyroid peroxidase
- secretion is inhibited by high levels of thyroid hormone
- TRH
- thyrotropin releasing hormone is produced in the hypothalamus
- secreted into the hypophyseal portal system and is transported to the anterior pituitary
- stimulates TSH secretion
- Physiologic Actions of Thyroid Hormone
- regulates heat production by increasing oxygen consumption and elevating the basal metabolic rate
- essential for normal growth and development
- affects protein, lipid, and carbohydrate metabolism
- increases GI motility
- increases the sensitivity of the sympathetic nervous system to the effects of catecholamines
Thyroid Function Tests
- TSH
- single most valuable test
- may detect hypothyroidism (↑ TSH) or hyperthyroidism (↓ TSH) before it is clinically apparent
- Total T4
- measures thyroid production
- will be elevated in hyperthyroidism and decreased in hypothyroidism
- measures free and bound hormone levels, which can be affected by the availability of thyroid-binding proteins
- Free T4, T3
- measures biologically active thyroid hormone
- Thyroid Antibodies
- produced in autoimmune thyroid disorders such as Hashimoto’s thyroiditis and Graves’ Disease
- may allow earlier detection of Graves’ disease and more accurate monitoring of the effects of antithyroid medications
- Serum Thyroglobulin
- most useful for monitoring thyroid cancer patients for recurrence after total thyroidectomy and RAI ablation
- Calcitonin
- can be used as a screening test in MEN2 kindreds or in any patient in whom medullary carcinoma of the thyroid is suspected
Thyroid Imaging
- Radioactive Iodine Scan
- directly evaluates thyroid gland function
- much less widely used now because of accurate measurements of TSH, T4, T3, and improved thyroid ultrasound
- used primarily to distinguish between causes of hyperthyroidism – solitary nodule vs diffuse goiter
- also used to detect thyroid cancer metastases after remnant thyroid radioactive ablation
- Ultrasound
- should be considered as an extension of the physical exam
- valuable in evaluating thyroid nodules: size, cystic vs solid, characteristics concerning for malignancy
(borders, presence of calcifications, vascularity)
- FNA
- key diagnostic modality in the workup of thyroid nodules
- size of the nodule and ultrasound characteristics are used to determine which nodules to biopsy
- ultrasound-guided biopsy yields more diagnostic specimens than freehand biopsies
- FNA analyzes cellular features, but not tissue architecture
- FNA is extremely accurate in diagnosing papillary thyroid cancer
- FNA cannot diagnose follicular cancer, since this requires demonstration of capsular or vascular invasion
- FNA has a false-negative rate between 1% - 6%
References
- Sabiston, 20th ed., pgs 881 – 889
- Schwartz, 10th ed., pgs 1521 - 1530
- O’Leary, pgs 312 – 317
- Simmons and Steed, pgs 288 - 291