Liver and Small Bowel Transplantation
Liver Transplantation (OLT)
- Indications
- Cholestatic Liver Disease
- Primary Biliary Cirrhosis
- autoimmune disorder that damages intralobular bile ducts
- post-transplant results are excellent: 90% - 95% 1-year survival
- disease recurrence (30%) is unlikely to require retransplant
- Primary Sclerosing Cholangitis
- affects the large intrahepatic and extrahepatic bile ducts
- majority of patients are males with ulcerative colitis
- associated with cholangiocarcinoma
- Alcoholic Liver Disease
- excellent 1-year results
- incidence of recidivism is ~ 10%
- most centers require a period of abstinence (6 months) prior to transplantation
- Chronic Hepatitis
- Hepatitis B
- used to be a contraindication for transplant because of rapid reinfection of the graft
- effective antiviral therapy and hyperimmune globulin has largely eradicated
reinfection after transplantation
- Hepatitis C
- most common indication in the West
- associated with worse outcomes than other indications for transplantation
- reinfection rate is 90% and may be unresponsive to alpha-interferon therapy
- pretreatment with interferon and ribavirin is effective, but is often not tolerated
in cirrhotic patients
- Malignancy
- HCC patients are eligible for OLT if they cannot tolerate a resection because of advanced
cirrhosis, and if they meet the Milan criteria
- patients who meet the Milan criteria are given extra priority for transplantation
- Milan Criteria
- single lesion ≤ 5 cm or up to 3 separate lesions all < 3 cm
- no gross vascular invasion
- no regional nodal or distant metastases
- Metabolic Diseases
- many metabolic diseases and inborn errors of metabolism may be cured by OLT
- examples include: Wilson’s disease, alpha1-antitrypsin disease, hemochromatosis
- Nonalcoholic Steatohepatitis
- associated with obesity and metabolic syndrome
- most common indication in some centers
- Biliary Atresia
- most common indication in the pediatric population
- majority of infants who undergo hepaticojejunostomy (Kasai procedure) will eventually
require OLT
- Fulminant Hepatic Failure
- often secondary to a hepatotoxin (acetaminophen) or fulminant viral infection
- patients are given the highest priority on the transplant list (status 1)
- it is difficult to predict who will recover with supportive therapy and who will benefit
from an OLT
- Contraindications
- Insufficient Cardiopulmonary Reserve
- patients should have a normal ejection fraction
- patients with severe CAD may require revascularization pretransplant
- oxygen-dependent COPD is a contraindication, as is refractory pulmonary hypertension
- Infections
- uncontrolled bacterial and fungal infections are absolute contraindications
- HIV infection is not a contraindication for most centers if the virus is controlled
- Malignancy
- Metastatic HCC is an absolute contraindication
- Patients with a prior treated malignancy (non-HCC) must be considered cured
- Psychosocial Issues
- patients must have the financial and psychological capacity to care for the transplanted organ
- continued drug or alcohol abuse is an absolute contraindication to OLT
- lack of commitment to immunosuppressive drugs is an absolute contraindication
- Recipient Criteria for OLT
- Decompensated Cirrhosis
- historic indication for OLT is decompensated cirrhosis manifested by hepatic encephalopathy,
ascites, portal hypertensive bleeding, hepatorenal syndrome, or subacute bacterial peritonitis
- has been replaced by the MELD score
- MELD Score
- reflects the likelihood of dying from cirrhosis within 3 months
- formula based on objective criteria that can be verified: creatine, bilirubin, INR, Na
- allows livers to be directed towards the sickest patients
- patients with a MELD score ≥ 15 are candidates for a liver transplant
- the transplant evaluation should begin when the MELD score is > 10
- multiple conditions exist that qualify for MELD exception points
- patients with fulminant hepatic failure have the highest priority (status 1), which
supersedes MELD score
- Operative Procedure
- Recipient Hepatectomy
- formidable procedure in patients with extensive portal hypertension
- requires simultaneous occlusion of both the IVC and portal veins
- anhepatic phase of the surgery refers to the period of time in which the new liver is being
sewn in, and is characterized by hemodynamic instability and increased variceal bleeding
- Venovenous Bypass
- used in patients who cannot tolerate the anhepatic phase
- improves venous return to the heart and minimizes mesenteric congestion
- blood is removed via the femoral and portal veins, and returned via the subclavian vein
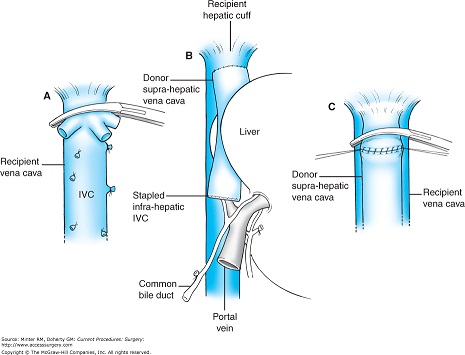
- Implantation
- usually performed in the orthotopic position
- suprahepatic caval anastomosis is performed first, followed by the infrahepatic caval
anastomosis
- portal vein anastomosis is performed next, followed by the hepatic artery anastomosis
- methods of biliary reconstruction include choledochocholedochostomy and
Roux-en-Y choledochojejunostomy
- Additional Techniques
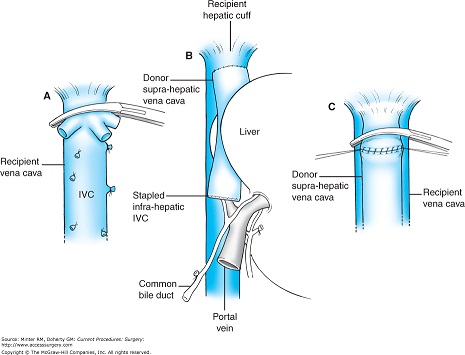
- Piggyback Technique
- recipient IVC is left intact and the liver is dissected off it
- all hepatic vein branches to the IVC are ligated except the three major hepatic veins
- orifices of the hepatic veins are then connected to form a common channel, which is
then anastomosed to the donor suprahepatic IVC
- advantages of this technique include avoidance of one vascular anastomosis and IVC
blood flow can be restored after completion of the suprahepatic caval anastomosis
- shortens the anhepatic phase and improves cardiovascular stability
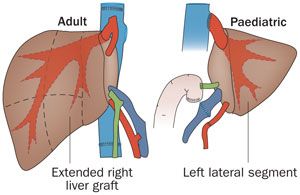
- Split-Liver Transplantation
- left lateral segment (segments 2, 3) is used in a child; the remaining segments are used
for an adult
- donor vessels supplying the liver remain with the right lobe
- pediatric graft is based on the left hepatic artery, left portal vein, and the left
hepatic vein
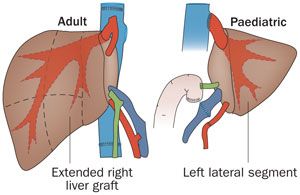
- Living-Related Transplantation
- typically from a parent to a child
- utilizes the donor’s left lateral segment
- major risk is morbidity and possible mortality (0.2%) to the donor
- Postoperative Management
- Immunosuppression
- maintenance therapy consists of a combination of a calcineurin inhibitor (tacrolimus), steroids,
and antiproliferative agent (mycophenolate mofetil)
- need for immunosuppression decreases over time
- chronic rejection is uncommon
- Acute Rejection
- occurs in 20% of patients, but rarely results in graft loss
- suspected by an elevation of liver enzymes (GGT, alkaline phosphatase, bilirubin)
- Doppler ultrasound is used to rule out hepatic artery thrombosis and bile duct obstruction
- diagnosis is made histologically by percutaneous liver biopsy
- usually responds to bolus steroid therapy or sirolimus
- Technical Complications
- Hepatic Artery Thrombosis
- more common in the pediatric population
- presents as a rapid rise in serum transaminase levels
- diagnosed by Doppler ultrasound
- treatment consists of revision of the anastomosis or retransplantation
- Portal Vein Thrombosis
- clinical manifestations may include a rising serum ammonia level, ascites, or variceal
bleeding
- diagnosis is made by Doppler ultrasound
- treatment is emergency thrombectomy and/or revision of the anastomosis
- Biliary Complications
- leaks and strictures occur in 10% to 35% of patients, most likely due to vascular compromise
- diagnosis is made by cholangiography
- leaks usually require reoperation and surgical correction
- strictures can usually be managed endoscopically or radiologically
Small Bowel Transplantation
- Indications
- irreversible intestinal failure combined with TPN failure
- small bowel transplants may also be combined with other organs, most commonly liver
- Intestinal Failure
- great majority of patients have short-gut syndrome as a result of extensive small bowel
resection
- common indications in adults include: Crohn’s disease, mesenteric thrombosis, and trauma
- common indications in children include: necrotizing enterocolitis, volvulus, intestinal
atresia, and gastroschisis
- intestinal failure is not defined based on a specific length of remaining bowel; but in
practical terms, results when > 75% of the gut is resected or nonfunctional
- TPN Failure
- TPN is associated with multiple potentially fatal complications
- cholestasis can lead to liver failure, especially in the pediatric population
- multiple central line infections or any fungal infection represents TPN failure
- multiple central vein thromboses is another criteria for TPN failure
- Donor Criteria
- must have a compatible blood type
- since loss of abdominal domain is common in recipients who have had an extensive resection, the
ideal donor would have a body weight 50% - 75% that of the recipient
- cold ischemia time must be minimized because it can lead to loss of mucosal integrity with resulting
increased bacterial translocation or intestinal perforation in the early post-op period
- Surgical Procedures
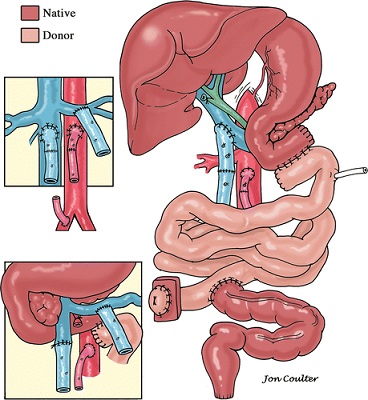
- Isolated Small Intestinal Transplant
- includes the entire jejunum and ileum
- arterial inflow is from the donor SMA to the recipient infrarenal aorta
- venous outflow is from the donor SMV to the recipient portal vein (preferred) or IVC
- donor arterial or venous conduits may be necessary to create the anastomoses
- bowel continuity is established proximally through anastomosis of the donor jejunum to the
recipient duodenum
- distal bowel continuity is established from the donor terminal ileum to the recipient’s
terminal ileum or colon
- a distal ileostomy (end or loop) is created to allow monitoring of the graft
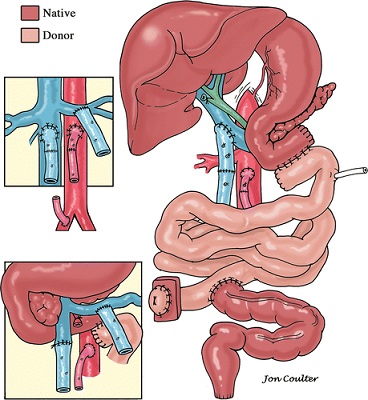
- Combined Small Bowel and Liver Transplants
- several possible options
- the grafts may come from the same donor, but are implanted separately
- another option is when the liver, intestine, duodenum, and pancreas are procured and
transplanted en bloc
- the en bloc procedure eliminates biliary reconstruction, which almost totally avoids
postoperative biliary complications
- Immunologic Considerations
- the intestine is highly immunogenic because of its abundant lymphoid tissue
- high levels of immunosuppression are required
- rejection rate is highest among all the solid organ transplants
- Immunosuppression
- induction is with a polyclonal T-cell antibody and high-dose steroids
- tacrolimus is the primary maintenance drug, along with prednisone
- Diagnosis of Rejection
- detected primarily by clinical symptoms, which mimic gastroenteritis, and graft histology
- symptoms include fever, abdominal pain, ileus, increased stomal output, elevated white blood
cell count
- serum citrulline and stool calprotectin are useful markers for rejection
- intestinal biopsies through the ileostomy may show cryptitis, shortening of villi,
mononuclear infiltrates, or mucosal sloughing
- liver transplants appear to have a protective effect for intestinal rejection
- Posttransplant Lymphoproliferative Disorder (PTLD)
- incidence is high at 10% - 20% of transplant recipients
- associated with Epstein-Barr virus infection, often from an EBV-positive donor to an
EBV-negative recipient
- initial treatment includes reduction of immunosuppression and antiviral medication
- chemotherapy may be required for Burkitt or T-cell lymphoma
- mortality rate is 25% - 60%
- Graft-versus-Host Disease
- donor lymphoid cells attack recipient tissues
- treatment involves increasing immunosuppression, which increases the infection risk
- mortality rate is high in severe cases
- Surgical Complications
- complication rate is ~ 50%
- most common technical complications include anastomotic leaks, intestinal perforations, and
intraabdominal abscesses
- signs and symptoms are often masked by high levels of immunosuppression
- graft thrombosis usually results in graft loss
References
- Sabiston, 20th ed., pgs 637 – 646, 666 – 674
- Schwartz, 10th ed. pgs 345 - 354
- UpToDate. Liver Transplantation in Adults: Patient Selection and Pretransplant Evaluation.
Lorna M. Dove, MD, MPH, Robert S. Brown, Jr., MD, MPH. Mar 26, 2021. Pgs 1 – 26
- UpToDate. Overview of Intestinal and Multivisceral Transplantation. Farrukh A. Khan, MD, FACS, Gennaro Selvaggi, MD.
Sep 16, 2020. Pgs 1 – 21