Primary Survey (ABCDE)
- Airway with Cervical Spine Protection (A)
- inadequate delivery of oxygenated blood to the brain and other vital structures is the quickest
killer of the injured patient
- prevention of hypoxia requires a protected, unobstructed airway and adequate ventilation
- airway and ventilation take priority over all other conditions
- Clinical Assessment
- if the patient is able to communicate verbally, the airway is not likely to be in immediate
jeopardy
- frequent reassessment of airway patency and adequacy of ventilation are critical
- rapid assessment of airway obstruction should include inspection for foreign bodies (teeth
and blood) and facial, mandibular, and laryngeal fractures
- tachypnea may be an early sign of airway obstruction
- patients who refuse to lie down may be having difficulty maintaining their airway
- look to see if the patient is agitated or obtunded:
- agitation suggests hypoxia
- obtundation suggests hypercarbia
- cyanosis of the nail beds or circumoral skin implies hypoxemia
- retractions and the use of accessory muscles suggests airway compromise
- listen for abnormal sounds:
- noisy breathing is obstructed breathing
- snoring, gurgling, and stridor may be associated with partial occlusion of the
larynx
- hoarseness implies obstruction of the larynx
- an abusive or belligerent patient may be hypoxic
- feel for the location of the trachea and determine if it is midline
- chin lift or jaw thrust are the initial maneuvers to establish a patent airway
- C-spine must be protected while assessing and managing the airway – manually stabilize the
patient’s head and neck using inline mobilization techniques
- C-Spine Protection
- spinal cord must be protected until spinal injury has been ruled out by clinical assessment
and/or imaging
- removal of helmets and collars is a two-person job (one person provides manual in-line
immobilization while the other removes the helmet or collar)
- in-line immobilization is mandatory during all procedures to maintain or obtain an airway
- Supplemental Oxygen
- should be administered immediately to all trauma patients
- Airway Maintenance Techniques
- tongue may fall backwards and obstruct the hypopharynx if the patient has a decreased level
of consciousness
- this form of obstruction can be corrected by the chin lift or jaw thrust maneuvers and
maintained with an oropharyngeal or nasopharyngeal airway
- Oropharyngeal Airway
- cannot be used in a conscious patient because it will induce gagging, vomiting,
and aspiration
- when inserting, must be careful not to push the tongue backward and block the airway
- Nasopharyngeal Airway
- better tolerated in a responsive patient
- Laryngeal Mask Airway (LMA)
- not a definitive airway
- useful if intubation has failed, or is unlikely to succeed
- requires appropriate training
- if an LMA is in place, must make plans for a definitive airway
- intubating LMA (ILMA) is a device that allows for intubation through the LMA
- Additional Airway devices
- laryngeal tube airway
- multilumen esophageal airway
- Definitive Airway
- Definition
- requires a tube present in the trachea with the cuff inflated, the tube connected to
some form of oxygen-enriched assisted ventilation, and the airway secured in place
with tape
- 3 varieties: orotracheal tube, nasotracheal tube, cricothyroidotomy
- Indications
- apnea
- inability to maintain a patent airway by other means
- airway protection from blood and vomitus
- impending airway compromise:
- large or expanding neck hematoma
- laryngeal/tracheal injury
- maxillofacial trauma (especially bilateral mandible fractures)
- facial burns
- inhalation injury
- closed head injury with GCS < 8
- inadequate oxygenation
- inadequate ventilation
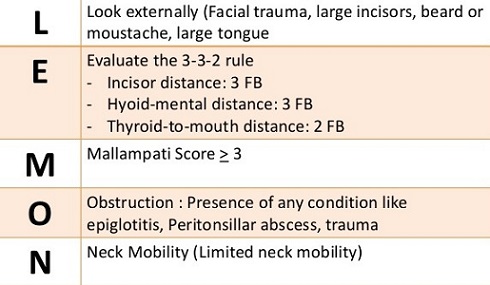
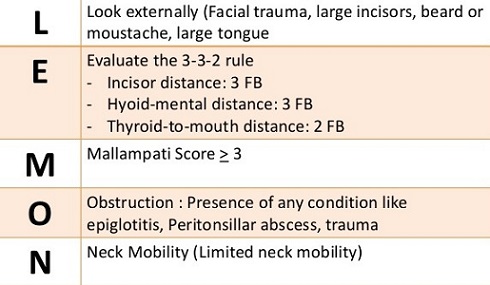
- LEMON Airway Assessment
- used to predict the difficulty of intubation
- Techniques
- Orotracheal Intubation
- most commonly chosen technique
- can be performed rapidly under direct vision
- suitable in both awake and apneic patients
- 2-person technique with in-line cervical spine immobilization should be used
- drug-assisted technique may be used in responsive patients
(succinylcholine/Etomidate), cricoid pressure
- if the cords can’t be visualized on laryngoscopy, a gum elastic bougie often
facilitates a successful intubation
- after intubation the chest and abdomen should be auscultated for equal
bilateral breath sounds
- CO2 monitor confirms proper intubation of the airway
- CXR is necessary to confirm proper positioning of the tube in the airway
- Nasotracheal Intubation
- blind technique requiring a spontaneously breathing patient
- contraindicated in apneic patients and patients with severe maxillofacial
trauma and basilar skull fractures
- most appropriate in hemodynamically stable patients with C-spine injuries
since less neck manipulation is required
- Cricothyroidotomy
- indicated when orotracheal and nasotracheal intubation is unsuccessful or
contraindicated
- must be performed with the neck in the neutral position
- easier, quicker, and associated with less bleeding than emergency
tracheostomy
- percutaneous tracheostomy should not be done because the patient’s neck must
be hyperextended
- should be converted to a formal tracheostomy as soon as the patient is
stable
- not recommended for children < 12 years’ old
- Jet Insufflation (Needle Cricothyroidotomy)
- provides oxygen on a short-term basis until a definitive airway can be placed
- 12- or 14-guage IV catheter is placed through the cricothyroid membrane into
the trachea
- catheter is then connected to high-flow (15 L/min) wall oxygen
- to provide ventilation, a hole is cut in the oxygen tubing and the hole is
covered for 1 second and uncovered for 4 seconds
- some exhalation occurs in the 4 seconds that oxygen isn’t flowing
- adequate oxygenation can only be maintained for 30 to 45 minutes
- CO2 slowly accumulates, further limiting the usefulness of this
method
- Breathing and Ventilation (B)
- Clinical Assessment
- airway patency does not assure adequate ventilation
- ventilation requires adequate functioning of the CNS, lungs, chest wall, and diaphragm, as
well as a patent airway
- look for symmetric and adequate chest wall excursion
- asymmetry suggests splinting or a flail chest
- labored breathing implies an imminent threat to the patient’s oxygenation
- listen for movement of air on both sides of the chest
- decreased or absent breath sounds over one or both hemithoraces indicates a thoracic
injury
- patients should be monitored with a pulse oximeter (monitors oxygenation, not ventilation)
- life-threatening thoracic injuries such as tension pneumothorax, open pneumothorax, and
massive hemothorax should be treated immediately
- Life Threating Emergencies
- Tension Pneumothorax
- Pathophysiology
- ‘one-way valve’ air leak occurs either from the lung or through the chest
wall
- air is forced into the thoracic cavity without any means of escape
- ipsilateral lung collapses and as the thoracic pressure increases, the
mediastinum is shifted to the opposite side, decreasing venous return
- Diagnosis
- clinical diagnosis: hypotension, respiratory distress, tracheal deviation,
neck vein distention, unilateral absence of breath sounds
- may be difficult to distinguish from cardiac tamponade
- Management
- immediate decompression with a large-bore needle into the 5th intercostal
space just anterior to the midaxillary line or finger thoracostomy
- converts the injury into a simple pneumothorax
- definitive treatment requires insertion of a chest tube
- Open Pneumothorax (‘Sucking Chest Wound’)
- Pathophysiology
- if a defect in the chest wall is greater than 2/3 the diameter of the
trachea, then air will follow the path of least resistance and pass
preferentially through the chest defect, rather than the mouth, with each
respiration
- result is impaired ventilation, leading to hypoxia and hypercarbia
- Management
- wound is covered with a sterile occlusive dressing and taped securely on
three sides
- goal is to create a flutter-type valve: as the patient breathes in,
the dressing is sucked over the wound, preventing air from escaping
- when the patient breathes out, the open end of the dressing allows air to
escape
- if the dressing is taped on all 4 sides, air can accumulate in the thoracic
cavity, resulting in a tension pneumothorax
- a chest tube should be placed remote from the wound as soon as possible
- definitive surgical closure of the defect is often required
- Flail Chest
- Pathophysiology
- segment of the chest wall does not have bony continuity with the rest of the
thoracic cage
- results when 2 or more ribs are fractured in 2 or more places
- the unstable segment moves paradoxically during respiration
- major insult in flail chest results from the underlying pulmonary contusion,
not the chest wall instability
- associated pain with restricted chest wall motion also contributes to
hypoxia
- Diagnosis
- physical exam will show paradoxical chest wall movement
- chest x-ray will show multiple rib fractures
- Management
- goal is to treat and/or prevent hypoxia
- many patients will require intubation and mechanical ventilation to
maintain an acceptable PO2
- aggressive pulmonary toilet and pain management (consider epidural catheter
or intercostal rib blocks) are the other cornerstones of management
- open reduction/internal fixation of the flail segment is rarely warranted
- Massive Hemothorax
- Mechanism of Injury
- results from the rapid accumulation of 1000 - 1500 cc of blood in the chest
cavity
- may result from blunt or penetrating trauma
- usually results from a systemic arterial (intercostal, internal mammary) or
pulmonary hilar injury
- since the lung is a low-pressure system, bleeding from the lung parenchyma
does not cause massive hemothorax
- Diagnosis
- hypovolemic shock associated with absence of breath sounds and/or dullness
to percussion on one side of the chest
- chest x-ray shows a large fluid collection
- Management
- insertion of a chest tube (28 – 32 F) that is connected to an autotransfusion
device
- restoration of blood volume with crystalloid and blood
- most patients with initial blood loss >1500 cc will require thoracotomy
- patients with ongoing blood loss of 250 cc/hr for 3 hours are also likely to
need thoracotomy
- patient’s physiologic status is the best guide for the need for surgery
- Cardiac Tamponade
- Pathophysiology
- most commonly results from penetrating injuries
- pericardial sac is a fixed fibrous structure that does not distend and as
little as 150 cc of blood may impair diastolic filling
- Diagnosis
- can be difficult in the trauma setting
- Beck’s triad (present in 1/3 of cases): 1) distended neck veins, 2) muffled
heart sounds, 3) hypotension
- Kussmaul’s sign: rise in venous pressure with inspiration when breathing
spontaneously
- tension pneumothorax can mimic tamponade
- pulseless electrical activity (PEA) in the absence of hypovolemia and
tension pneumothorax suggests cardiac tamponade
- FAST is a valuable non-invasive tool for showing fluid in the pericardial
sac (false-negative rate = 5%)
- Management
- volume resuscitation will transiently improve cardiac output
- subxiphoid pericardiocentesis is both diagnostic and therapeutic
- patients with a positive pericardiocentesis or FAST exam will require
thoracotomy or sternotomy for definitive repair of the heart
- Role of ER Thoracotomy
- patients with penetrating chest injuries who arrive pulseless, but with myocardial
electrical activity, may be candidates for immediate resuscitative thoracotomy
- patients sustaining blunt injuries who arrive pulseless are not candidates for ER
thoracotomy
- therapeutic maneuvers that can be accomplished with ER thoracotomy include:
- release of pericardial tamponade
- direct control of exsanguinating hemorrhage
- open cardiac massage
- cross-clamping of the descending aorta to slow blood loss below the
diaphragm and increase perfusion to the brain and heart
- Circulation with Hemorrhage Control (C)
- hemorrhage is the main cause of early death following injury
- hypotension following injury is hypovolemic in origin until proven otherwise
- bleeding will be from one or more of 5 locations: chest, abdomen, retroperitoneum
(often pelvic fractures), long bones, and external sites
- Clinical Assessment
- tachycardia is the earliest physiologic response to blood loss
- cutaneous vasoconstriction is another early sign of blood loss
- systolic blood pressure may not fall until 30% of the blood volume has been lost
- altered level of consciousness as a result of decreased cerebral perfusion accompanies
profound blood loss
- acute blood loss cannot reliably be estimated using the hemoglobin or hematocrit
concentration
- CXR to evaluate for thoracic bleeding
- pelvic x-ray to identify pelvic fractures
- FAST, DPL to evaluate for intra-abdominal bleeding
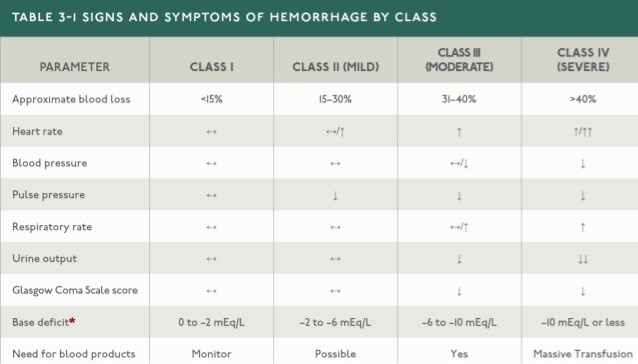
- ATLS Classification of Hemorrhagic Shock
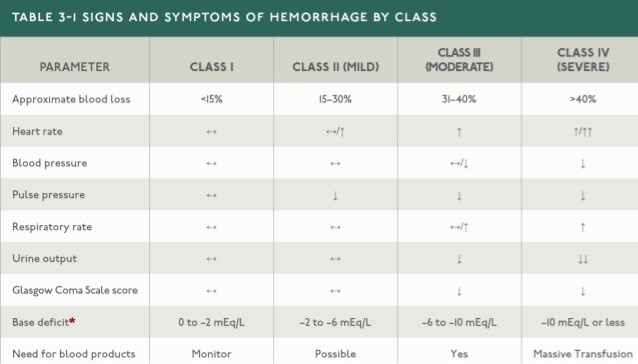
- athletes (conditioning), elderly patients (medications), and pregnant patients
(hypervolemia) may deviate from this classification
- Control of Blood Loss
- external blood loss is managed by direct manual pressure on the wound
- pelvic binder or pneumatic antishock garment may be used to control bleeding from pelvic
fractures
- long bone fractures should be splinted
- chest tube for intrathoracic bleeding
- Resuscitation
- Vascular Access
- 2 large-bore peripheral IVs should be started immediately
- if peripheral access cannot be obtained, central lines, cutdowns, or intraosseous
infusion can be used
- Initial Resuscitation
- blood should be sent immediately for type and crossmatch
- adults should receive an initial fluid bolus of one liter
- if the patient remains hypotensive, O-negative, type-specific, or type and
crossmatched blood should be given, depending upon their availability
- consider autotransfusion in any patient with a major hemothorax
- all IV fluids and blood products should be warmed to prevent hypothermia
- Massive Transfusion
- a small subset of patients will require massive transfusion (> 10 units PRBCs in
24 hours)
- goal is to minimize excessive crystalloid infusion
- PRBCs, FFP, and platelets are given in a balanced ratio (often 1:1:1)
- simultaneously, the source of bleeding must be controlled as fast as possible
- Coagulopathy
- consumption of coagulation factors, dilution, hypothermia, and acidosis all
contribute to coagulopathy
- many patients are also taking antiplatelet or anticoagulation drugs
- baseline PT, PTT, and platelet count should be obtained early
- prothrombin complex concentrate can be used to reverse Coumadin
- tranexamic acid – an antifibrinolytic agent – administered within 3 hours of injury
improves survival
- Disability (D)
- the goal of management is to maintain cerebral perfusion and oxygenation, thereby preventing
secondary brain injury
- a rapid neurological exam is performed at the end of the primary survey
- patient’s level of consciousness as well as pupil size and reactivity should also be assessed
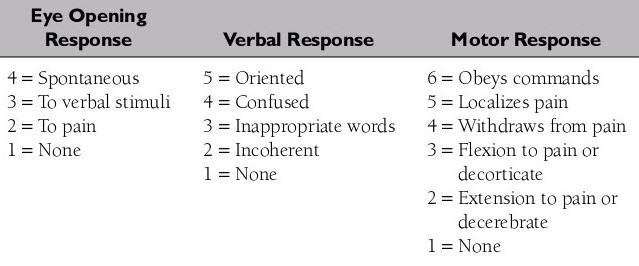
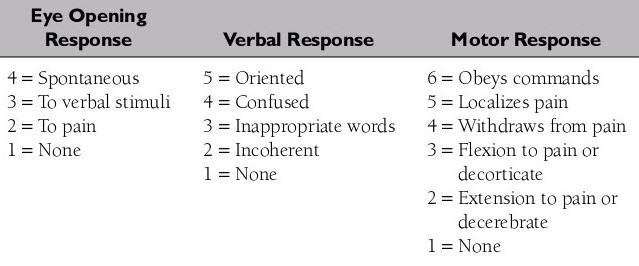
- Glasgow Coma Scale (GCS) is a quick neurological evaluation that is predictive of patient outcome
(motor response)
- Exposure and Environmental Control (E)
- patient must be completely exposed to facilitate a thorough examination
- after the patient has been assessed, then he must be covered with warm blankets or an external
warming device to prevent hypothermia
- the trauma room should be warm
- all IV fluids and blood products should be warmed before infusion
- Adjuncts to the Primary Survey
- EKG Monitoring
- required of all trauma patients to detect dysrhythmias
- Pulse Oximeter
- measures the oxygen saturation and heart rate
- Blood Pressure Monitor
- automated device is used and frequently cycled
- Urinary Catheter
- urinary output is a sensitive indicator of volume status and reflects renal perfusion
- transurethral catheter placement is contraindicated if urethral transection is suspected:
- blood at the penile meatus
- perineal ecchymosis
- blood in the scrotum
- pelvic fracture
- if urethral injury is suspected, then a retrograde urethrogram must be performed before the
catheter is inserted
- Nasogastric Tube
- purpose is to decrease gastric distention and reduce the risk of aspiration
- if a fracture of the cribriform plate is suspected, then the tube should be inserted orally
to prevent intracranial passage
- insertion of the gastric catheter may induce gagging and vomiting and cause the specific
problem it was intended to prevent: aspiration
- X-rays and Diagnostic Studies
- X-rays
- Chest X-ray
- should be obtained in all patients with blunt or penetrating torso trauma or who are
in respiratory distress
- additional indications include any unconscious patient or any patient going to the
operating room
- Pelvic X-ray
- should be obtained in any patient sustaining blunt trauma to the torso
- additional indications include gross hematuria, gross blood on rectal or vaginal
examination, and unexplained hypotension
- Diagnostic Studies
- Diagnostic Peritoneal Lavage (DPL)
- 98% sensitive for intraperitoneal bleeding
- used in hemodynamically unstable blunt trauma patients if FAST is not available
- only absolute contraindication is an existing indication for laparotomy
- relative contraindications include previous abdominal surgery, morbid obesity, and
coagulopathy
- Diagnostic Ultrasound (FAST)
- as accurate as DPL for detecting hemoperitoneum, and has largely replaced DPL in
most trauma centers
- requires special training
- may be repeated at intervals to detect progressive hemoperitoneum
Secondary Survey
- History
- allergies, medicines, past and current illnesses, previous surgery, and the events surrounding
the injury and mechanism of injury are the critical elements of the history
- family members and prehospital personnel often have to provide these details
- Physical Examination
- the patient must be completely examined: head and skull, maxillofacial, neck, chest, abdomen,
perineum/rectum/vagina, musculoskeletal, and a complete neurological examination
- ‘a finger in every orifice’
- Adjuncts to the Secondary Survey
- specialized tests may be performed to identify specific injuries: CT scans, angiograms, endoscopy,
ultrasound, extremity x-rays, additional c-spine views
- no specialized test should be performed until the patient has been fully examined and his
hemodynamic status has normalized
References
- ATLS Student Course Manual 2012, 9th ed., Pgs 2 – 60
- ATLS Student Course Manual 2018, 10th ed., pgs 2 - 61
- Cameron, 13th ed., pgs 1105 - 1111, 1124 - 1131