Anatomy
- Scalp
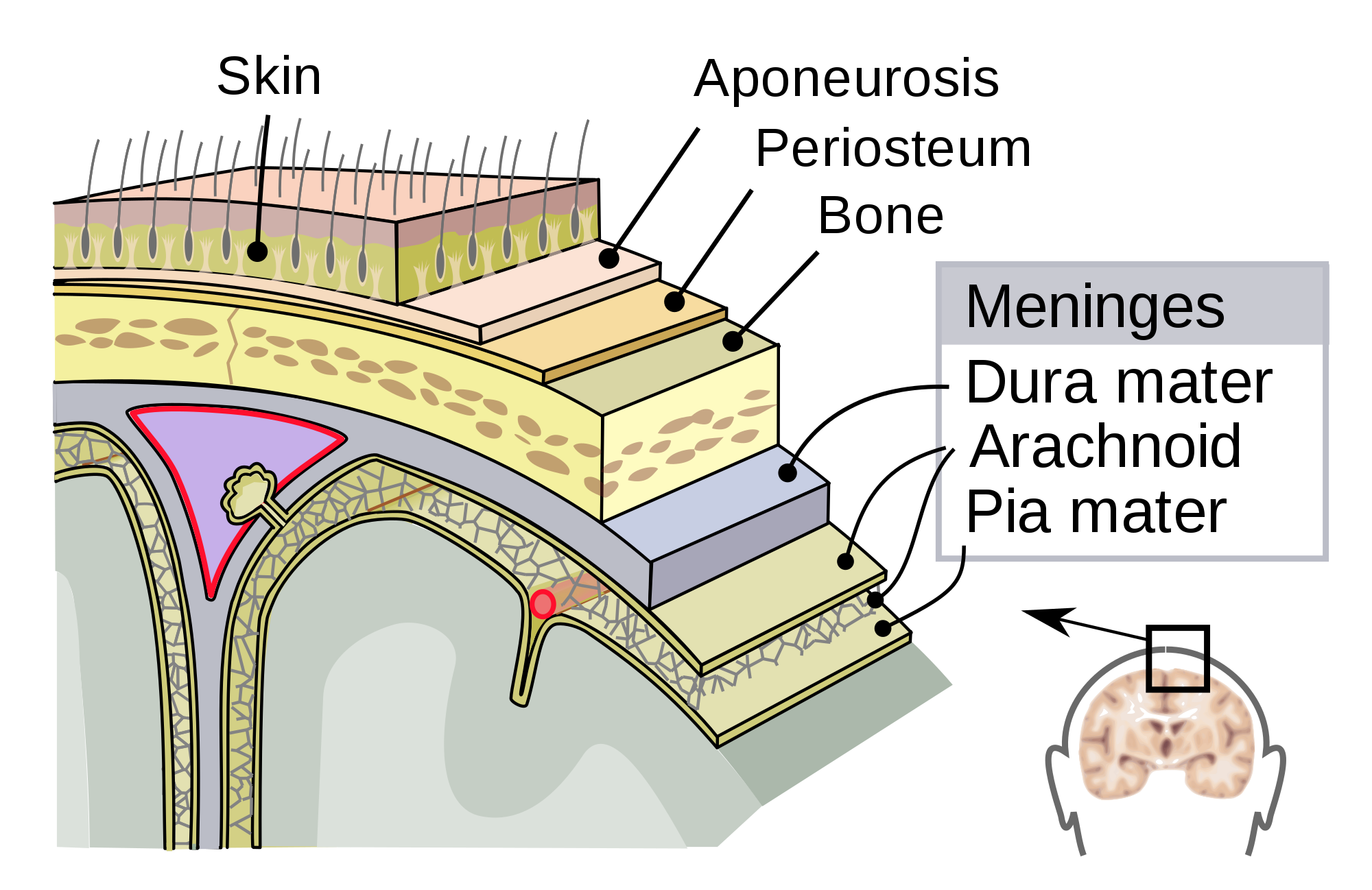
- composed of 5 layers (mnemonic SCALP):
- Skin
- Connective tissue
- Aponeurosis (galea)
- Loose connective tissue
- Pericranium
- because the scalp has such a generous blood supply, scalp lacerations can result in major blood
loss, especially in infants and children
- initial management of a bleeding scalp laceration is to apply a pressure dressing
- large hematomas can collect below the galea
- the galea should be repaired when closing scalp lacerations
- Skull
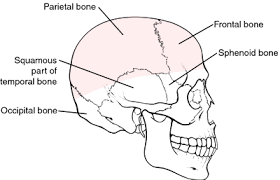
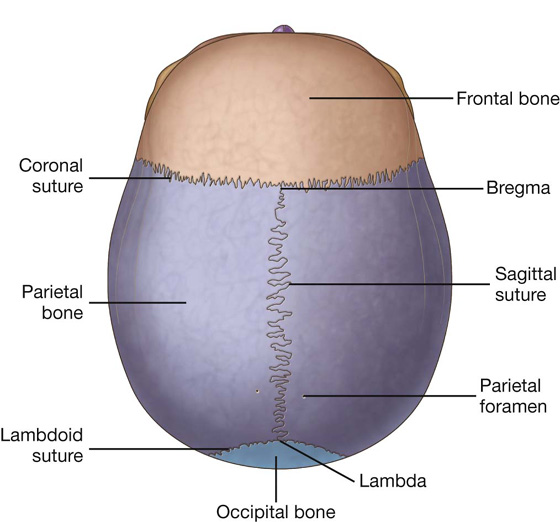
- composed of the cranial vault (calvaria) and the base
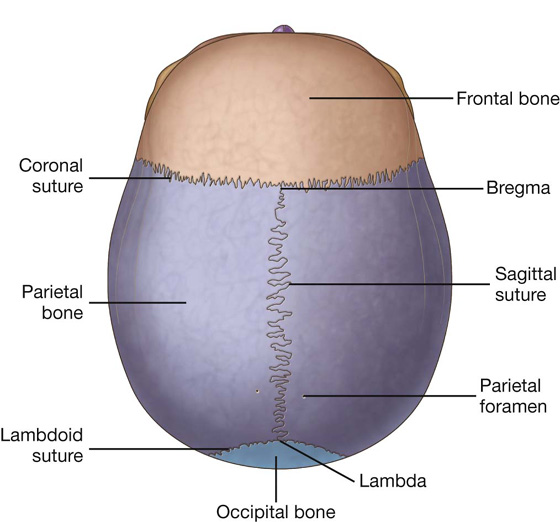
- Calvaria
- formed anteriorly by the frontal bone and posteriorly by the parietal and occipital bones
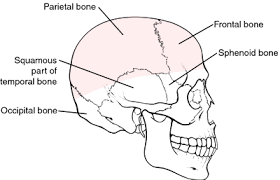
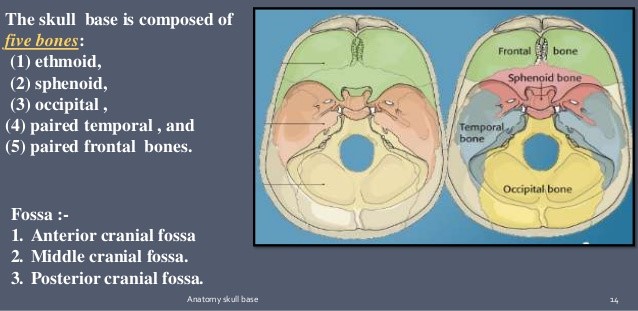
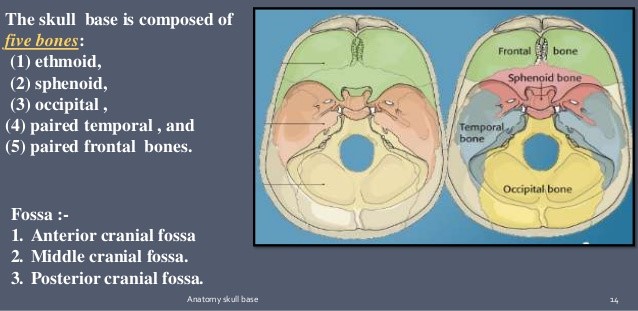
- Base
- formed by the frontal, ethmoid, sphenoid, temporal, and occipital bones
- floor of the skull base is divided into anterior, middle, and posterior fossa
- cranial nerves exit the skull via foramina located in the skull base
- Meninges
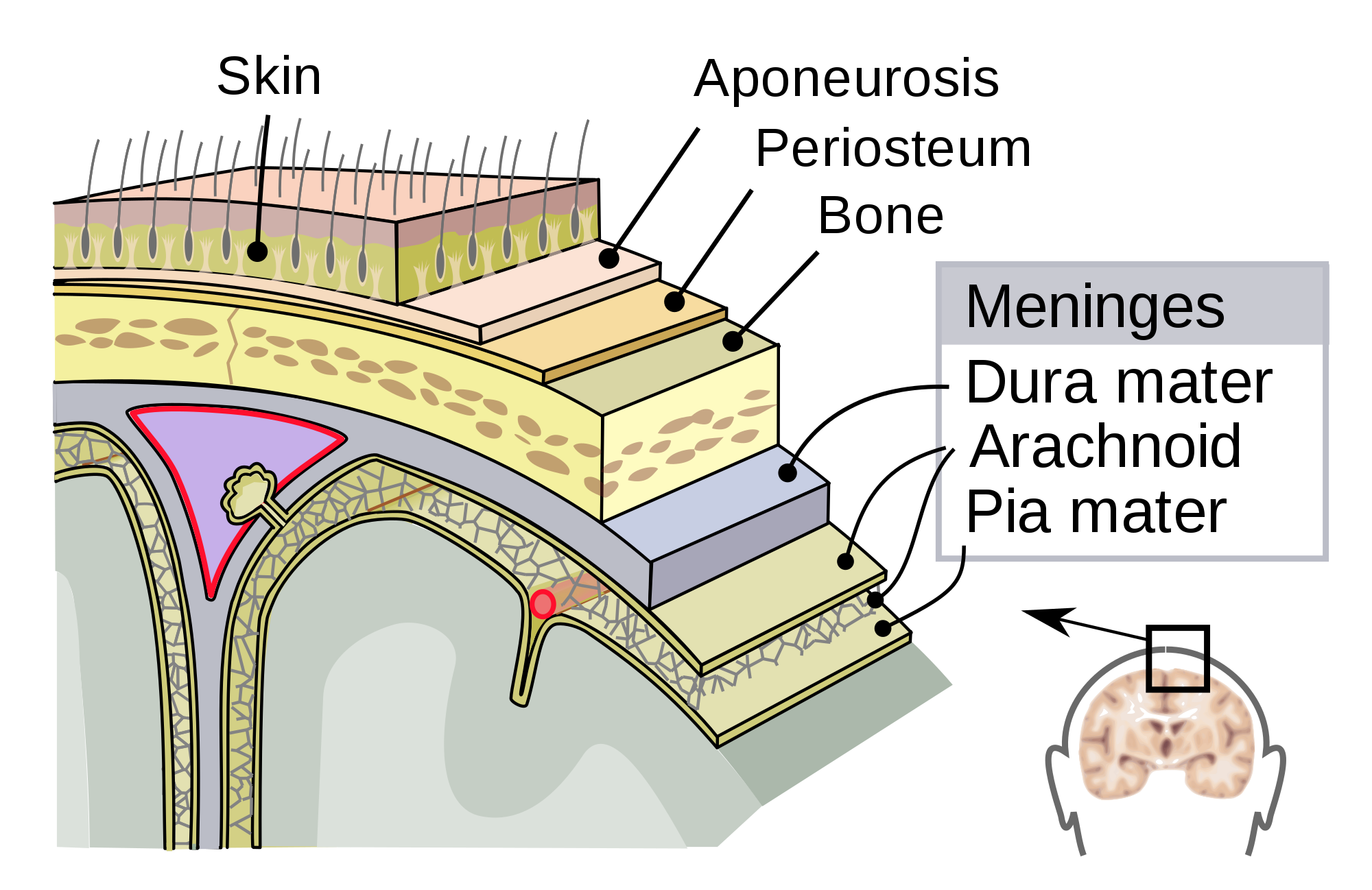
- Dura Mater
- tough fibrous membrane that adheres firmly to the internal surface of the skull
- meningeal arteries lie between the dura and the skull (epidural space)
- because the dura is not attached to the underlying arachnoid, a potential space
(subdural space) exists into which hemorrhage can occur
- dura encloses the large venous sinuses that provide the venous drainage for the brain
(superior sagittal, transverse, sigmoid sinuses)
- Arachnoid
- thin, transparent layer
- cerebrospinal fluid (CSF) circulates between the arachnoid and pia mater
- head trauma may cause accumulation of blood in this space (subarachnoid hemorrhage)
- Pia Mater
- firmly attached to the surface of the brain
- Brain
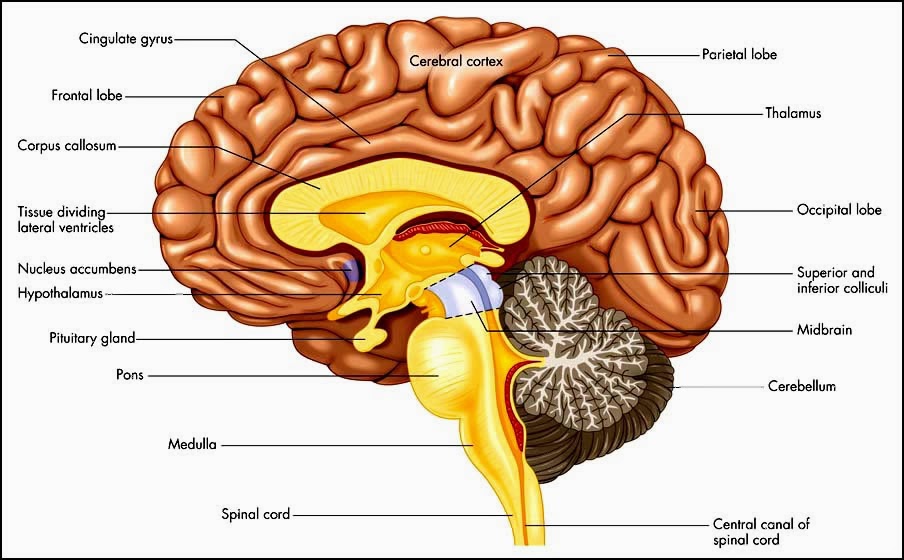
- Cerebrum
- composed of right and left hemispheres separated by the falx cerebri, a dural reflection
from the inferior aspect of the superior sagittal sinus
- hemisphere that contains the language centers is referred to as the dominant hemisphere
(left hemisphere in virtually all right-handed people and 85% of left-handed people)
- cerebrum is composed of 4 lobes:
- frontal lobe: concerned with emotions, motor function, speech
- parietal lobe: concerned with sensory function and spatial orientation
- temporal lobe: concerned with speech, memory
- occipital lobe: concerned with vision
- Cerebellum
- responsible mainly for coordination and balance
- located in the posterior fossa
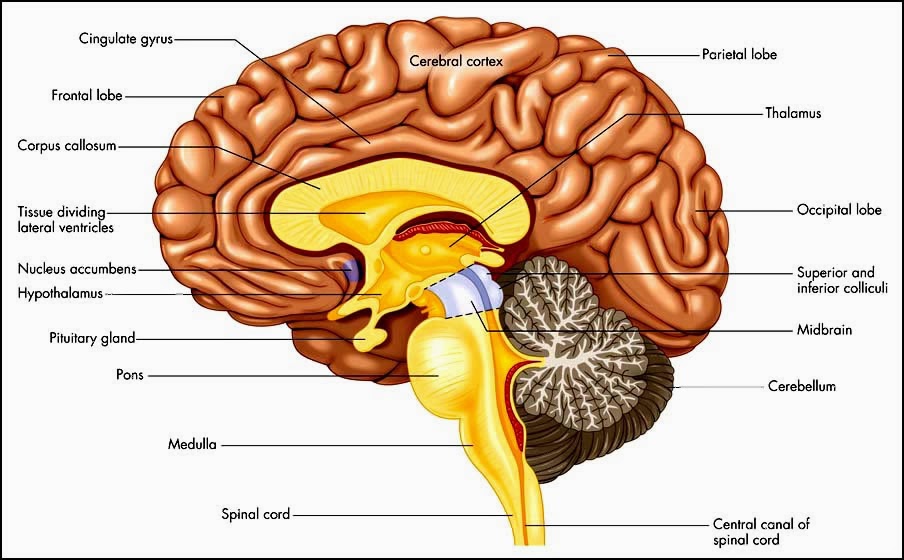
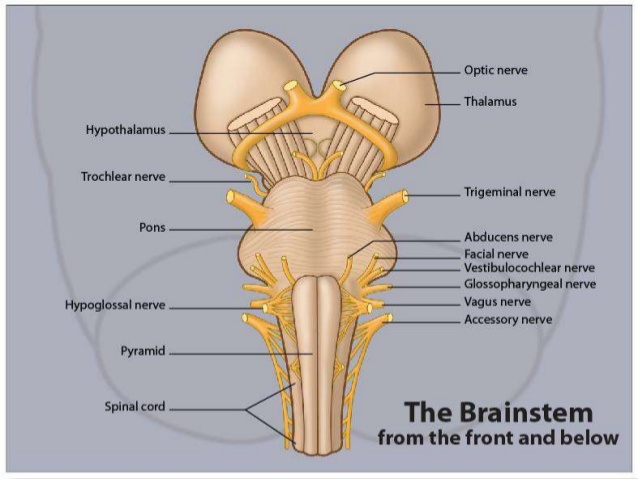
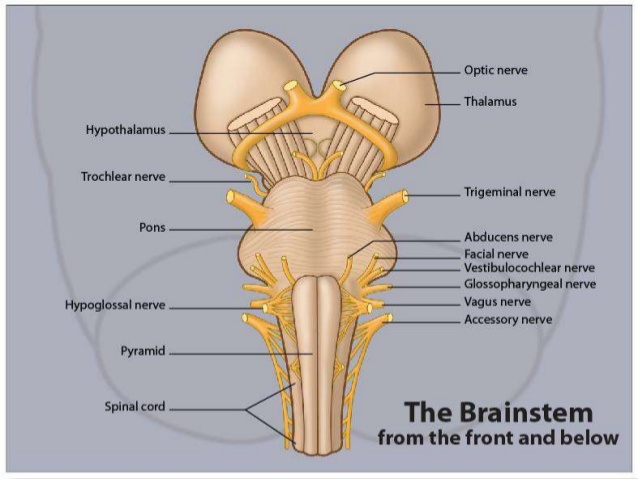
- Brainstem
- composed of the midbrain, pons, and medulla
- midbrain connects the cerebral hemispheres to the pons and medulla
- midbrain and upper pons contain the reticular activating system, which is responsible for
the state of alertness
- medulla contains vital cardiorespiratory centers
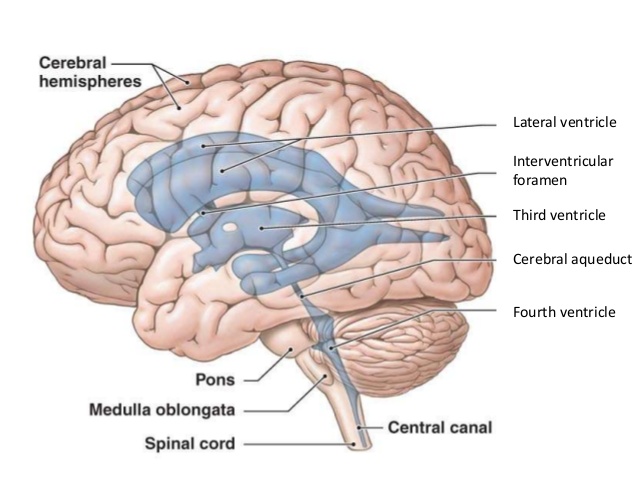
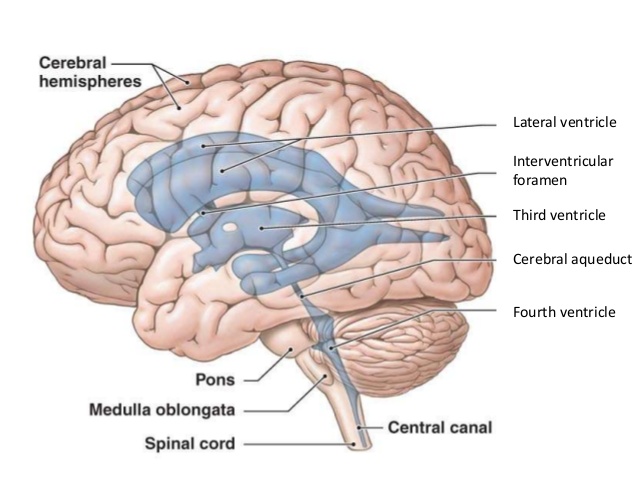
- Cerebrospinal Fluid
- produced by the choroid plexus, which is located in the lateral ventricles
- CSF travels from the lateral ventricles, through the foramen of Monro, into the 3rd ventricle,
and then, via the aqueduct of Sylvius, into the 4th ventricle
- CSF exits from the ventricular system into the subarachnoid space, where it is eventually reabsorbed
into the venous circulation through the arachnoid granulations that project into the superior sagittal sinus
- presence of blood in the CSF can plug the arachnoid granulations and impair CSF reabsorption,
leading to increased intracranial pressure (communicating hydrocephalus)
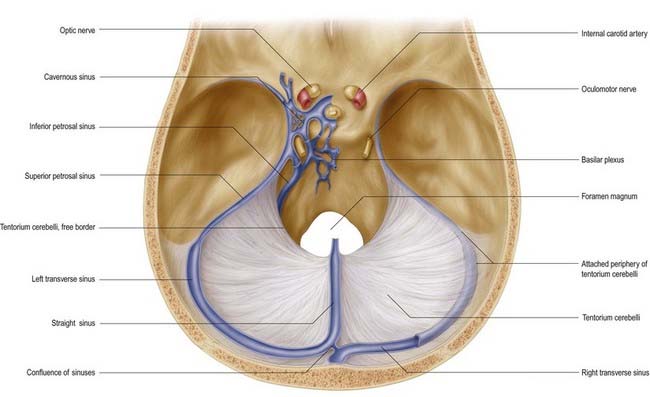
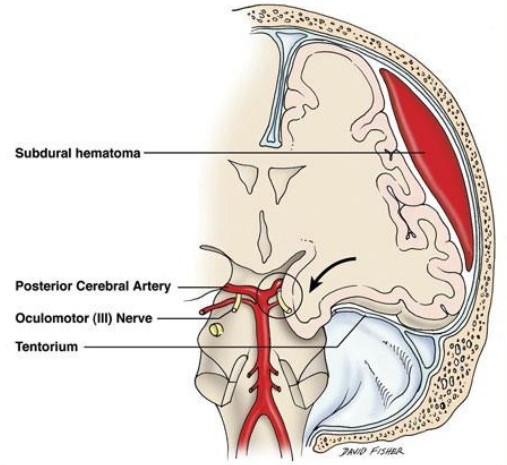
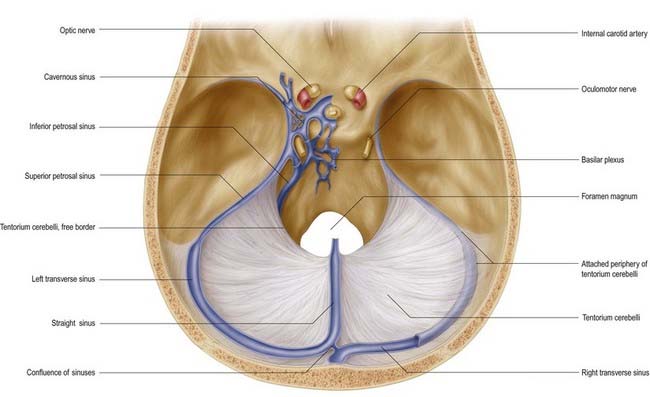
- Tentorium
- tentorium cerebelli divides the head into the supratentorial compartment (anterior + middle fossae)
and infratentorial compartment (posterior fossa)
- midbrain passes through a large opening in the tentorium known as the tentorial notch
- oculomotor nerve runs along the edge of the tentorium
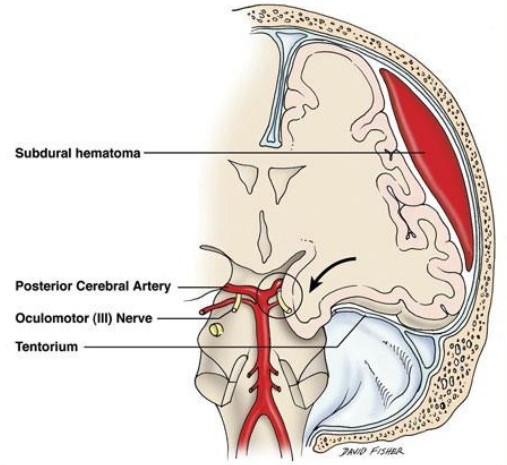
- Brain Herniation
- a supratentorial mass or edema may cause downward brain herniation through the tentorial notch
- medial part of the temporal lobe (uncus) is the part of the brain that usually herniates
- as the brain herniates downward, the oculomotor nerve becomes compressed against the tentorium
- parasympathetic fibers (pupillary constrictors) lie on the surface of the oculomotor nerve
- compression of these parasympathetic fibers leads to pupillary dilatation as a result of
unopposed sympathetic activity
- with further compression of the oculomotor nerve, full oculomotor paralysis occurs, causing the
eye to deviate inferiorly and laterally (‘down and out’)
- uncal herniation also causes compression of the corticospinal tract in the midbrain
- this motor tract crosses to the opposite side at the foramen magnum; therefore, compression of
the corticospinal tract results in weakness of the opposite side of the body
(contralateral hemiplegia)
- ipsilateral pupillary dilatation with contralateral hemiplegia is the classic syndrome of
tentorial herniation

Physiology
- Intracranial Pressure (ICP)
- normal ICP = 10 mm Hg
- ICP > 20 mm Hg is abnormal and ICP > 40 mm Hg is severely abnormal
- the higher the ICP following head injury, the worse the outcome
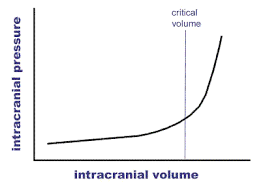
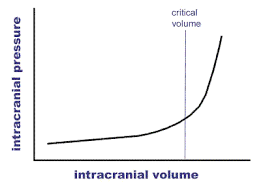
- Monro-Kellie Doctrine
- the cranial vault is a nonexpansile box
- within this box is the brain, CSF, venous blood, and arterial blood
- the total volume of the box must remain constant
- the addition of a mass or swelling will raise ICP unless an equal volume of CSF and venous
blood is squeezed out
- once this compensatory mechanism is exhausted, even a small increase in the size of the mass
will lead to an exponential increase in ICP:
- Cerebral Perfusion Pressure (CPP)
- CPP = MAP – ICP
- if ICP is elevated, then blood pressure must be maintained at normal or supranormal levels to
maintain CPP
- maintaining cerebral perfusion is of primary importance in the management of head injury patients
- Cerebral Blood Flow (CBF)
- autoregulation maintains a constant CBF between mean arterial pressures of 50 and 160 mm Hg
- below a MAP of 50 mm Hg, CBF declines significantly; above a MAP of 160 mm Hg, CBF increases
significantly
- autoregulation is often severely disturbed in head-injured patients
Classification of Injuries
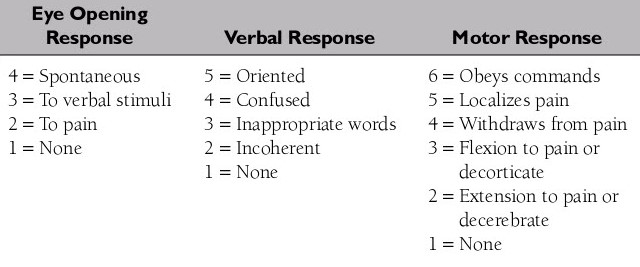
- Glasgow Coma Scale
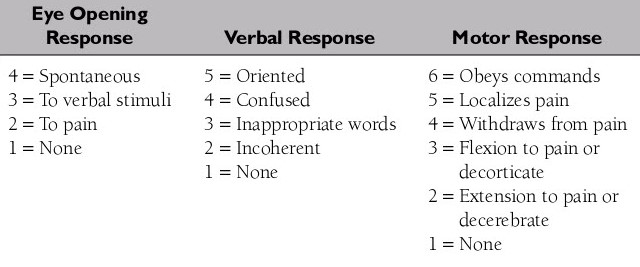
- Severity of Injury
- GCS score is used to quantify neurological findings and allows uniformity in description of patients
with head injury
- coma is defined as the inability to obey commands, utter words, and open the eyes
- severe head injury (coma) is defined as a GCS score between 3 and 8
- moderate head injury is a GCS score between 9 and 13
- mild head injury is a GCS score of 14 and 15
- Types of Injury
- Skull Fractures
- may be seen in the calvaria or skull base, may be open or closed, linear or stellate,
depressed or non-depressed
- basal skull fractures require CT scanning with bone windows for identification
- clinical signs of a basal skull fracture include periorbital ecchymosis (raccoon eyes),
retroauricular ecchymosis (Battle’s sign), CSF leaks (rhinorrhea, otorrhea), and VIIth nerve
palsy

- a linear skull fracture increases the risk of intracranial hematoma by 400 times in a
conscious patient and by 20 times in an unconscious patient
- depressed skull fractures require surgical elevation when the fragments are depressed more
than the thickness of the skull
- open skull fractures also require surgical repair since the dura is often torn, resulting in
a direct communication between the skin and cerebral surface
- Focal Intracranial Lesions
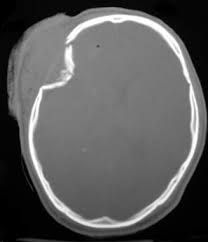
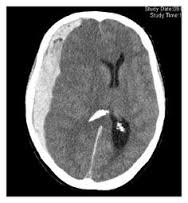
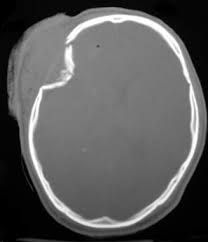
- Epidural Hematoma
- relatively uncommon (0.5% of all head-injured patients, 9% of comatose patients)
- most often located in the temporal or temporoparietal region
- most commonly results from a torn middle meningeal artery as a result of a skull
fracture
- 1/3 result from venous bleeding (torn venous sinuses)
- have a lenticular shape on CT scan
- patients may present with the classic lucent interval followed by rapid deterioration
(‘talk and die’)
- if recognized and treated early, prognosis is usually excellent because direct damage
to the underlying brain is often limited
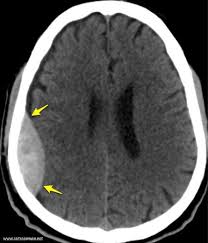
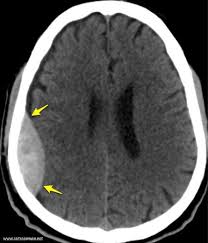
- Subdural Hematoma
- much more common than epidural hematomas (30% of severe head injuries)
- typically occurs as a result of tearing of the bridging veins between the cerebral
cortex and draining venous sinuses
- usually covers the entire surface of the cerebral hemisphere
- prognosis is much worse than for epidural hematomas because the underlying brain
injury is usually more severe
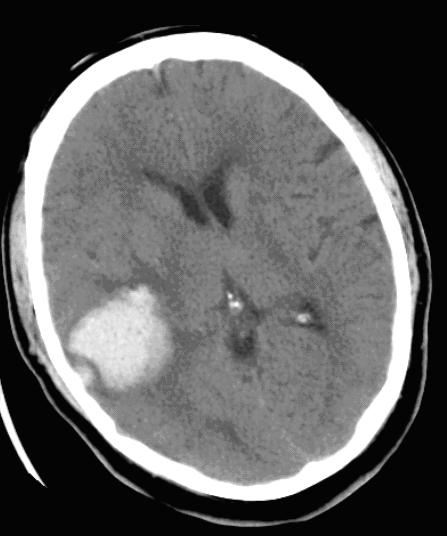
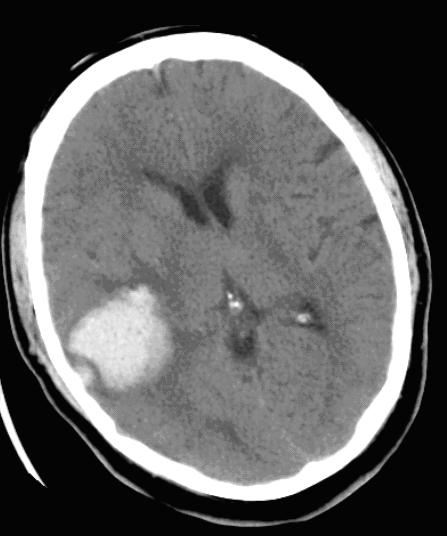
- Cerebral Contusions and Hematomas
- often associated with subdural hematomas
- most occur in the frontal and temporal lobes
- occur as a result of the brain hitting the undersurface of the skull
- small contusions may coalesce into larger hematomas
- large hematomas may require surgical evacuation because of mass effect
- Diffuse Brain Injuries
- represent a continuum of brain damage produced by increasing amounts of
acceleration-deceleration forces
- most common type of head injury
- Mild Concussion
- consciousness is preserved, but there is temporary neurological dysfunction
(confusion, disorientation without amnesia)
- syndrome is completely reversible
- Classic Concussion
- results in a loss of consciousness
- patients return to full consciousness within 6 hours
- accompanied by posttraumatic amnesia
- most patients have no sequelae other than amnesia for the event
- some patients develop post-concussion syndrome and have long-lasting neurologic
deficits (memory difficulties, dizziness, nausea, anosmia, depression)
- Diffuse Axonal Injury
- prolonged posttraumatic coma that is not due to a mass lesion or ischemic insult
- caused by a shearing injury to the axons
- head CT scan may appear normal
- recovery is difficult to predict and patients often remain severely disabled, if
they survive
Management of Head Trauma
- CT scan should be obtained on all head injury patients who report any loss of consciousness, amnesia to the
event, confusion, or severe headache
- Mild Head Injury (GCS 13 – 15)
- 80% of patients with head injury fall into this category
- patients are awake, but may report brief loss of consciousness or disorientation, amnesia to the
event, or severe headache
- GCS 13: 25% have CT evidence of trauma, and 1.3% will require neurosurgical intervention
- GCS 15: 10% have CT evidence of trauma, and 0.5% will require neurosurgical intervention
- patients who are awake/alert, asymptomatic, with no neurologic deficits may be discharged, ideally
to a companion who can observe them for another 24 hours
- patients who are symptomatic, or who have CT abnormalities, should be admitted and have a
neurosurgery consult
- Moderate Head Injury (GCS 9 – 12)
- patients are able to follow simple commands but usually are confused or somnolent
- may have focal deficits such as hemiparesis
- ~ 10% to 20% of patients deteriorate and lapse into coma
- 40% of patients will have an abnormal CT scan and 8% will require surgery
- patients should be admitted to the ICU and have frequent neuro status checks
- follow up CT in 24 hours, or any time that there is a change in neuro status
- avoid hypotension, hypoxia, hypoventilation
- Severe Head Injury (GCS 3 – 8)
- ABCDE
- Airway and Breathing
- brain injury is worsened by secondary insults (hypoxia, hypotension)
- securing a definitive airway is mandatory
- patient should be ventilated with 100% FiO2
- hyperventilation should be used cautiously and only when neurologic deterioration
has occurred
- aim for a PCO2 of 35 mm Hg initially
- Circulation
- hypotension should be corrected with aggressive use of isotonic fluids and blood
products
- aim for an SBP ≥ 100 mm Hg
- hypotension is assumed to be the result of severe blood loss, not the head injury
- every patient should undergo FAST exam to eliminate an abdominal source of bleeding
- if the patient remains hypotensive, then correction of the hypotension
(laparotomy, thoracotomy) takes precedence over the neurological evaluation
- if the patient becomes hemodynamically stable after resuscitation, then the first
priority is a head CT scan
- Neurological Exam
- rapid minineurologic exam (GCS score, pupillary light response, focal deficit) is
performed once the patient’s cardiopulmonary status has been stabilized
- alcohol, drugs can confound the neurologic assessment
- exam should be done prior to sedating or paralyzing the patient, if possible
- long-acting paralytic agents should be avoided
- motor responses can be elicited by nail bed or nipple pressure
- multiple serial exams should be performed in order to detect deterioration as early
as possible
- Diagnostic Procedures
- emergency CT scan of the head must be obtained as soon as possible
- the important CT findings are the presence of an intracranial hematoma, contusions,
midline shift (mass effect), obliteration of the basal cisterns
- a shift of 5 mm or greater usually indicates that surgery is needed
- Nonsurgical Management of Severe Head Injury
- IV fluids
- goal is to maintain normovolemia
- both dehydration and volume overload are harmful to the head-injured patient
- hypotonic fluids should be avoided
- must monitor serum sodium concentration (avoid hyponatremia, which can worsen brain
edema)
- avoid glucose-containing fluids, since hyperglycemia is harmful to the injured
brain
- normal saline or lactated Ringer’s should be used for resuscitation
- Correction of Anticoagulation
- reversal of aspirin and Plavix will require platelets and/or DDAVP
- Coumadin reversal will require vitamin K and/or prothrombin complex concentrate
(PCC, Kcentra)
- heparin and Lovenox may be reversed with protamine
- direct thrombin inhibitors (dabigatran, Pradaxa) can be reversed with idarucizumab
(Praxbind)
- factor Xa inhibitors (Xarelto) may be partially reversed with PCC
- Hyperventilation
- should be used cautiously
- ↓ PCO2 → ↑ cerebral vasoconstriction → ↓
intracranial volume → ↓ ICP
- however, too aggressive or prolonged hyperventilation can cause cerebral ischemia by
causing severe cerebral vasoconstriction
- PCO2 should be kept at 35 mm Hg
- brief periods of hyperventilation (PCO2 between 25 to 30 mm Hg) can be
used for acute neurological deterioration until other treatments are initiated
(surgery, e.g.)
- PCO2 > 45 should also be avoided, since it leads to cerebral vasodilation
and increased ICP
- Mannitol
- used to reduce ICP by causing an osmotic diuresis
- should not be given to a hypotensive patient since it can worsen hypovolemia and
cerebral ischemia
- given as a 1 g/kg IV bolus
- lasix is often used in conjunction with mannitol
- Hypertonic Saline
- concentrations of 3% to 23.4% are used
- may be preferable in hypotensive patients, since it does not act as a diuretic
- no evidence that it is superior to mannitol in lowering ICP
- Barbiturates
- effective in reducing ICP refractory to other methods
- since they can cause hypotension and cardiovascular depression, they should not be
used during resuscitation or in any hypotensive patient
- Anticonvulsants
- 15% of patients with severe head injury develop posttraumatic epilepsy
- prophylactic anticonvulsants reduce the incidence of seizures in the first week of
injury but not thereafter
- acute seizures must be controlled with anticonvulsants as soon as possible, since
prolonged seizures may cause secondary brain injury
- Steroids
- no beneficial effect in reducing ICP or improving outcome from severe head injury
- Emergency Surgical Management
- Depressed Skull Fractures
- will require elevation when the depth of depression is greater than the thickness of
the skull
- open skull fractures will require irrigation, debridement, dural closure, and
prophylactic antibiotics
- for less severe skull fractures, closure of the overlying scalp laceration is
indicated
- Intracranial Mass Lesions
- if a neurosurgeon is not available, the patient should be transferred as soon as
possible to a hospital with a neurosurgeon
- A CT scan is not required before transfer to definitive care
- if an intracranial hematoma is imminently life-threatening and there is no time for
transfer, emergency craniotomy or burr holes may be considered if someone adequately
trained in the procedure is available
- emergency procedures should only be done with the advice and consent of a neurosurgeon
- bone flap craniotomy is the definitive lifesaving procedure
- the burr hole should be placed on the side of the larger pupil
- Penetrating Brain Injuries
- CT scanning is strongly recommended
- when the trajectory is near the skull base or a major dural venous sinus, or if there is
substantial subarachnoid hemorrhage, then vascular imaging should be considered
- prophylactic antibiotics are appropriate
- Brain Death
- Clinical criteria
- GCS = 3
- nonreactive pupils
- absent brainstem reflexes (corneal, gag)
- no spontaneous ventilation during formal apnea testing
- absence of hypothermia or drug intoxication
- Ancillary Tests
- no EEG activity
- no cerebral blood flow (Doppler studies, angiography)
References
- ATLS Student Manual, 10th ed., pgs 102 - 126
- Cameron, 11th ed., pgs 1001 - 1005