Penetrating Neck Injuries
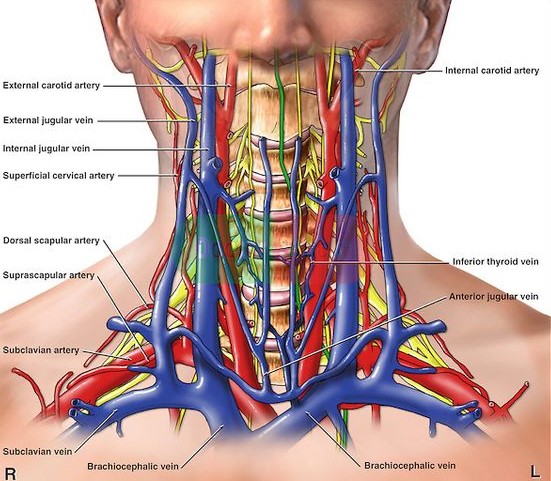
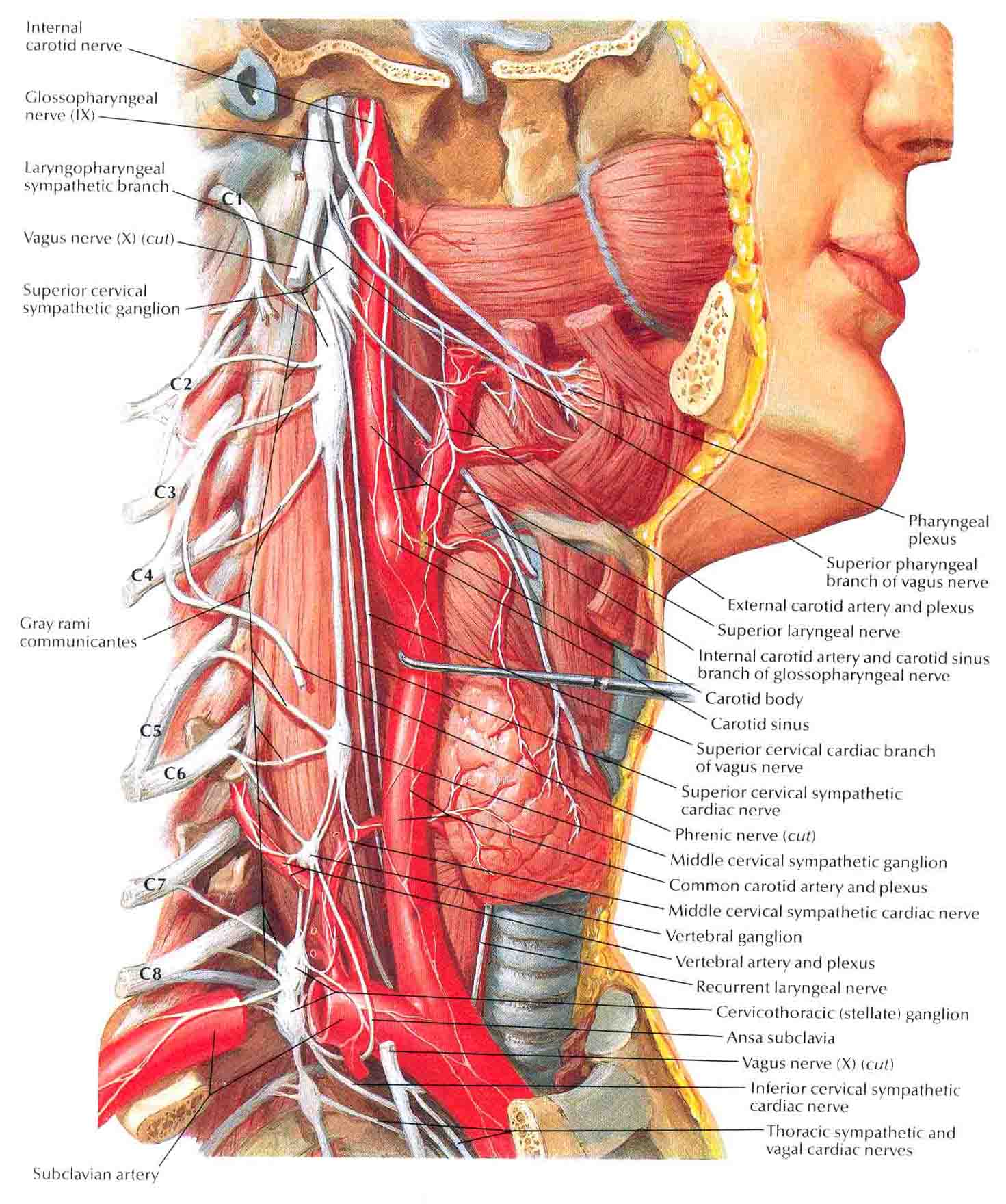
Anatomy and Zones
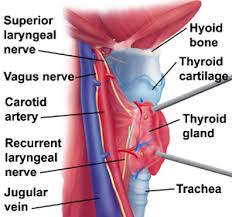
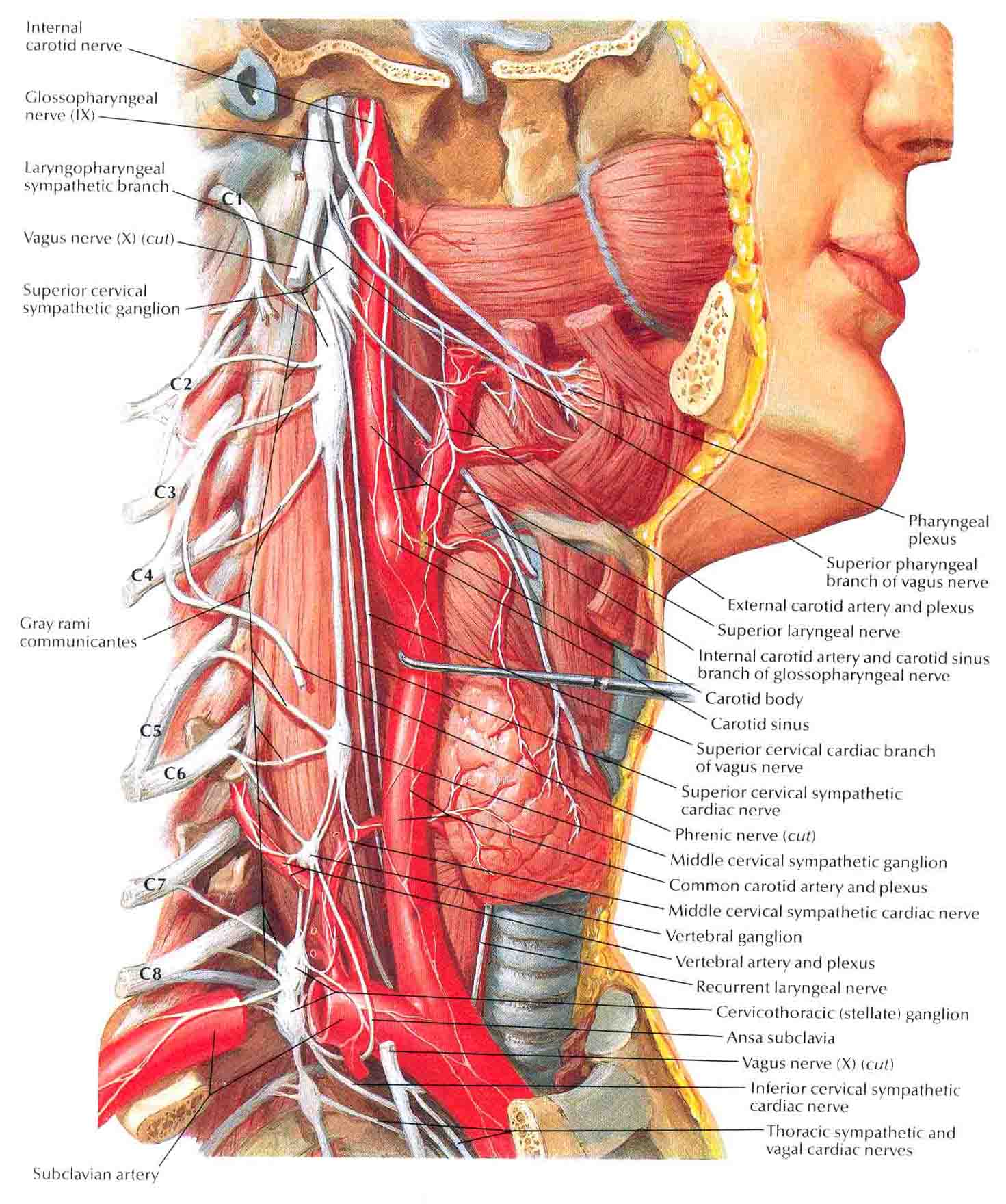
- Anatomy

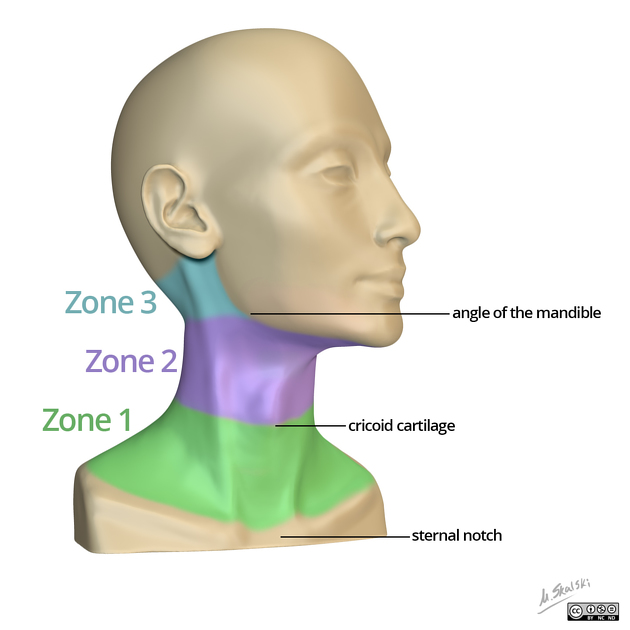
- Neck Zones
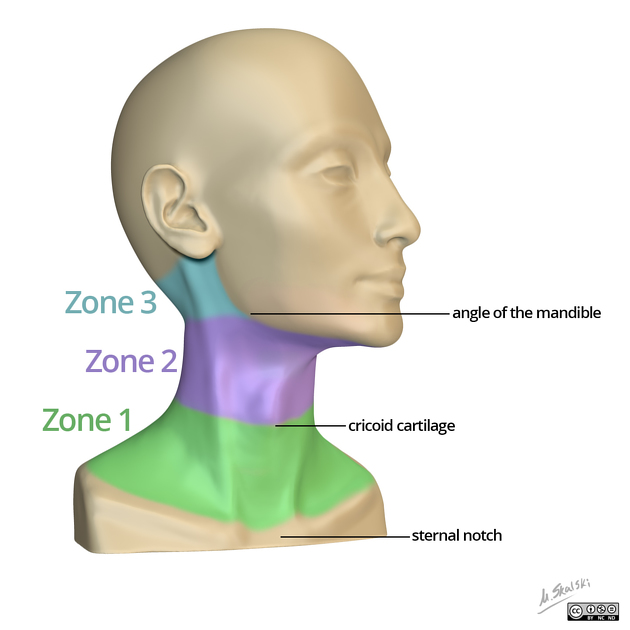
- Zone 1
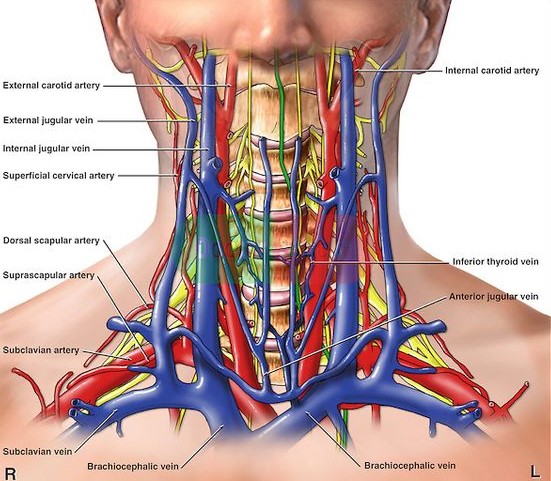
- extends from the clavicles to the cricoid cartilage
- surgical exposure is difficult: sternum, ribs, clavicle
- injuries have a high mortality rate from major vascular injury and intrathoracic injury
- structures traversing zone 1 include the great vessels, proximal carotid artery, vertebral
artery, lung, trachea, esophagus, spinal cord, major cervical nerve trunks
- Zone 2
- extends from the cricoid cartilage to the angle of the mandible
- surgical exposure is straightforward
- structures traversing zone 2 include the internal jugular vein, common, external, and
internal carotid arteries, vertebral artery, esophagus, trachea, larynx, hypopharynx,
spinal cord
- Zone 3
- extends from the angle of the mandible to the base of the skull
- surgical exposure is difficult because of the mandible and skull base
- structures traversing zone 3 include the jugular vein, distal internal carotid artery,
vertebral artery, pharynx
- Tissue Planes
- Platysma Muscle
- major anatomic landmark
- management decisions are made depending on whether the injury has penetrated this layer
- Deep Cervical Fascia
- supports and encircles the visceral and muscular structures of the neck
- tough layer that provides a natural tamponade effect in case of vascular injuries
- however, in a small closed space, this can result in extrinsic compression of the airway
Initial Management
- ABCDE
- assessing and securing the airway is the top priority
- significant external bleeding should be controlled with direct pressure: blind clamping of vessels
is to be avoided
- always consider the possibility of c-spine injury
- chest x-ray to rule out pneumothorax
- lateral c-spine x-ray to look for foreign bodies or subcutaneous air
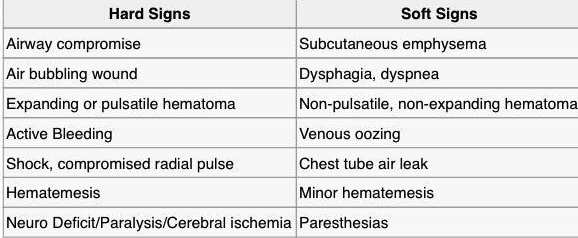
- Clinical Evaluation of the Neck
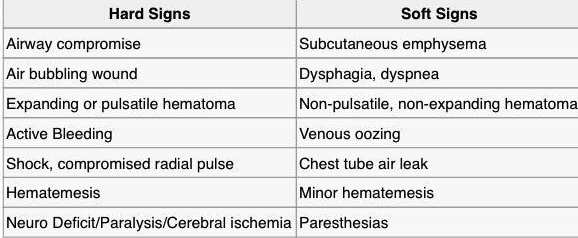
- physical findings are usually divided into hard and soft signs
- management decisions are based on the zone of injury and the presence of hard or soft signs of
injury
Management of Unstable Patients
- Zone 1 Injuries
- unstable patients belong in the operating room
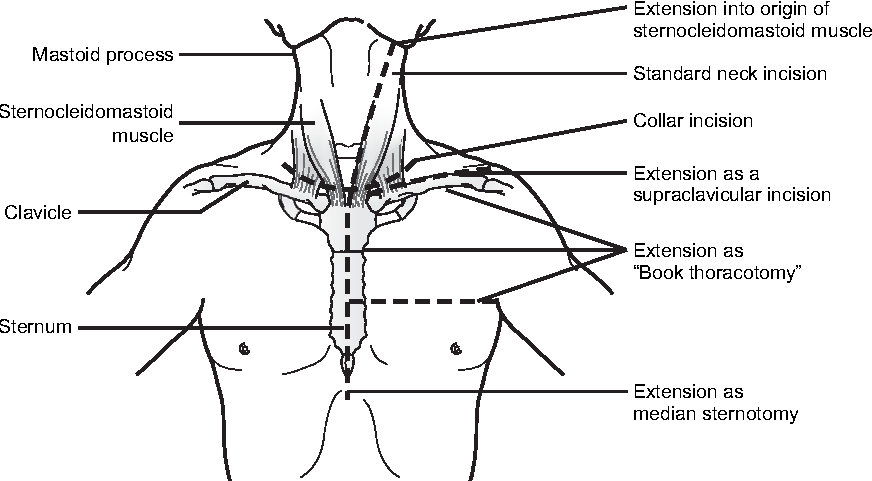
- choice of incision is based on what underlying vessel is injured
- possible incisions are supraclavicular, median sternotomy, anterolateral thoracotomy
- surgeon must be prepared to extend the initial incision or make additional incisions based on the
operative findings
- median sternotomy is used for exposure of the innominate, proximal right carotid and subclavian,
and proximal left carotid arteries
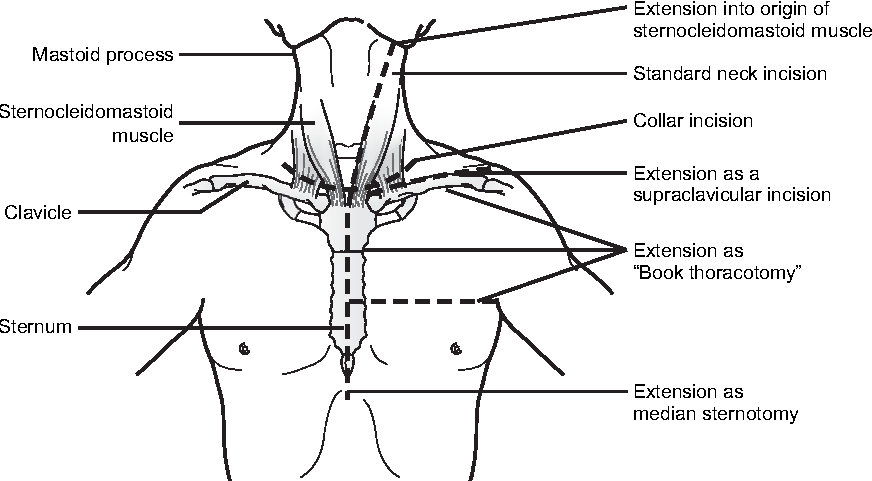
- Proximal Left Subclavian Artery Injuries
- proximal left subclavian artery is difficult to expose because it arises from the aortic
arch posteriorly
- a posterolateral thoracotomy provides excellent exposure but limits exposure to other vital
structures
- a ‘book’ thoracotomy provides the best exposure but is highly morbid: anterolateral
thoracotomy, supraclavicular incision with resection of the medial clavicle, and a median
sternotomy, which links the two horizontal incisions
- a proximal occlusion catheter may be placed to control hemorrhage prior to definitive repair
- Mid to Distal Left Subclavian Artery Injuries
- exposed by resecting the medial portion of the clavicle
- the artery lies posterior to the vein
- endovascular stent placement may be considered as definitive repair
- Zone 2 Injuries
- anterior sternocleidomastoid incision for unilateral injury
- transverse collar incision if both sides of the neck must be explored
- Internal Jugular Vein
- venorrhaphy for simple injuries
- patch venoplasty and segmental resection/primary anastomosis are also acceptable procedures
in stable patients
- extensive injuries or unstable patients should be managed with ligation
- bilateral ligation should be avoided (increased intracerebral pressure, facial swelling)
- Carotid Artery
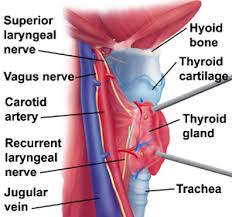
- common carotid is more frequently injured than the external or internal carotid
- common presentations include shock, expanding hematoma, brisk external bleeding, neurologic
deficit, coma
- ligation of the facial vein is required for adequate exposure
- must avoid injury to the adjacent vagus and hypoglossal nerves
- carotid artery repair is indicated in all patients except those with coma and no evidence of
prograde flow
- minor injuries can be repaired primarily
- complex injuries will require an interposition graft with autogenous vein or PTFE
- role of shunts remains controversial
- Vertebral Artery
- injury is usually not detected unless arteriography has been performed
- in a stable patient, expectant management is favored
- ongoing bleeding, arteriovenous fistula, or pseudoaneurysm is best managed by angiographic
embolization
- Esophagus
- there is significant morbidity and mortality for either a missed or delayed diagnosis of an
esophageal injury
- NG tube facilitates identification and dissection
- procedure of choice is debridement of devitalized tissues, primary repair, and wide drainage
- if the injury is extensive or if the diagnosis has been delayed for more than 24 – 48 hours,
then distal ligation and proximal esophagostomy is necessary
- Trachea
- simple lacerations may be repaired with an absorbable monofilament suture
- resection and end-to-end anastomosis can be performed for more extensive injuries as long as the
anastomosis is tension-free
- significant injuries will also require a tracheostomy, which may be placed above the level
of the injury
- Combined Tracheoesophageal Injuries
- each injury should be managed individually
- to avoid postop fistulas, a muscle flap (sternocleidomastoid or strap muscle) should be
interposed between the 2 suture lines
Management of Stable Patients
- Zone 1 Injuries
- management is selective
- CT angiography is performed to identify vascular injury
- esophageal injury is excluded by esophagography and esophagoscopy
- bronchoscopy is used to exclude injury to the trachea
- Zone 2 Injuries
- Mandatory Operative Intervention
- historically, any zone 2 injury that penetrated the platysma required operative exploration
- based on the experience in World War II, during which the mortality rate from penetrating
neck injuries was decreased by ~50% after adopting a mandatory neck exploration policy
- however, because of the high incidence of negative neck explorations, as well as better
diagnostic tools, this policy has become less common in recent years
- most people still recommend mandatory exploration for gunshot wounds
- Selective Management
- if there is no clinical evidence for injury to a vital structure, then
bronchoscopy/laryngoscopy, esophagoscopy/esophagography, and CT angiography are performed
- operation is performed only if an injury is detected by one of these studies
- since mortality rates do not appear to be less with this approach, it has become the most
common way to handle zone 2 neck injuries
- Zone 3 Injuries
- selective management is the rule because of the difficulty of operative exposure
- CT angiography is performed to rule out injury to the distal internal carotid
- most vascular injuries identified in zone 3 can be managed by endovascular stent placement
- esophageal studies are not necessary
References
- Cameron, 11th ed., pgs 1081 – 1085
- Sabiston, 20th ed., pgs 423 – 424