Overview
- trauma is the leading nonobstetric cause of maternal mortality
- most common mechanisms of injury are falls or MVAs
- pregnant women who sustain trauma have a higher incidence of
spontaneous abortion, preterm labor, fetomaternal hemorrhage, abruptio placentae,
and uterine rupture than age-matched pregnant controls
- best treatment for the fetus is optimal resuscitation of the mother
Anatomic and Physiologic Alterations of Pregnancy
- Anatomic Differences
- uterus remains intrapelvic until the 12th week, protected by the bony pelvis
- by 20 weeks, the uterus is at the umbilicus, and the bowel is being pushed cephalad
- by 34 – 36 weeks, the uterus reaches the costal margins
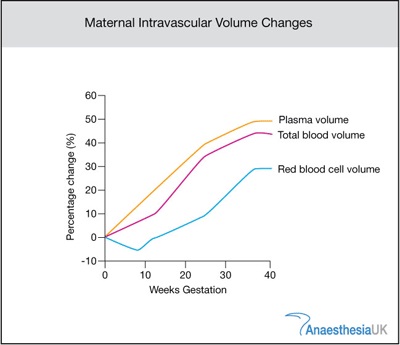
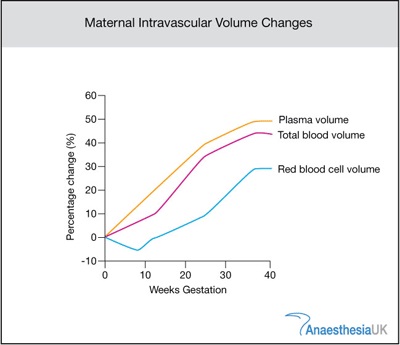
- Blood Volume and Composition
- plasma volume increases throughout pregnancy
- a smaller increase in RBC mass also occurs, resulting in a decreased hematocrit level
(physiologic anemia of pregnancy)
- in late pregnancy, a hematocrit level of 31% - 35% is normal
- a healthy pregnant woman can lose 30% of her blood volume (1200 – 1500 cc) before tachycardia and
hypotension ensue
- however, as a response to the blood loss, uterine vascular resistance greatly increases
- this results in decreased uterine blood flow and decreased fetal oxygenation
- thus, fluid resuscitation should be started early even in a normotensive pregnant trauma patient
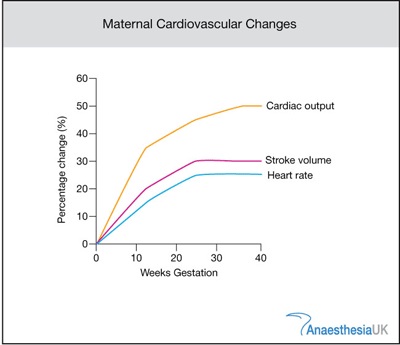
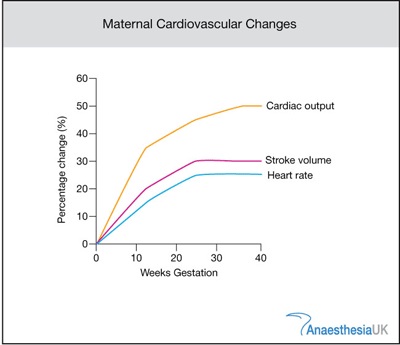
- Hemodynamics
- Cardiac Output
- cardiac output is increased in pregnancy, with the uterus and placenta receiving
20% of the cardiac output during the 3rd trimester
- however, in the supine position during late pregnancy, uterine compression of the
vena cava can decrease cardiac output by 30%
- pregnant trauma patients should be placed in the left lateral decubitus position
- if spinal cord injury is suspected, the patient may be secured to a backboard and then
tilted to the left
- Heart Rate, Blood Pressure
- heart rate increases by 10 – 15 beats/min during pregnancy
- SBP and DBP fall by 5 – 15 mm Hg
- these facts must be recognized when interpreting vital signs in a pregnant trauma patient
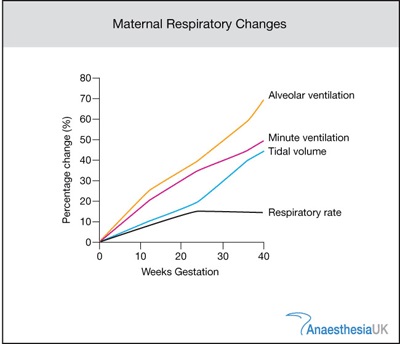
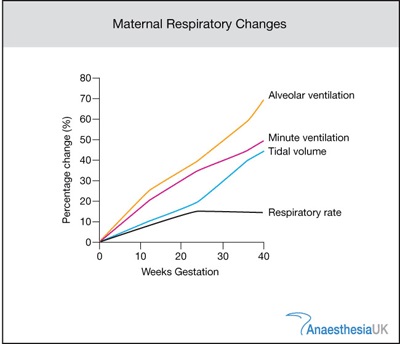
- Respiratory System
- minute ventilation increases during pregnancy
- PCO2 of 30 mm Hg during late pregnancy is normal
- PCO2 of 35 – 40 mm Hg may indicate impending respiratory failure during pregnancy
- oxygen consumption during pregnancy is increased
- it is imperative to maintain arterial oxygenation during resuscitation of injured pregnant patients
(aim for an oxygen saturation of 95%)
- Musculoskeletal System
- symphysis pubis widens to 4 – 8 mm
- sacroiliac joint spaces increase by the 7th month
- these factors must be kept in mind when interpreting pelvic x-rays
- Neurologic System
- eclampsia is a complication of late pregnancy that can mimic head injury
- neurological and obstetrical consultation may be necessary to help differentiate between
eclampsia and other causes of seizures
Primary Survey and Resuscitation
- ABCs
- always the first priority
- patient’s right side should be elevated by 15 – 30 degrees
- even with normal vital signs, aggressive fluid resuscitation is indicated to support the
hypervolemia of pregnancy
- vasopressors are an absolute last resort since they further reduce uterine blood flow, worsening
fetal hypoxia
- Abdominal Examination
- goal is to detect serious maternal injuries
- main cause of fetal death is maternal shock and maternal death
- indications for FAST and CT scan are the same as in nonpregnant patients
- if DPL is done, the catheter should be placed above the umbilicus using the open technique
- Pelvic Examination
- OB-GYN should be consulted early
- patient needs a formal pelvic examination, ideally by an OB-GYN
- significant findings include vaginal bleeding, amniotic fluid, cervical effacement and dilation,
fetal presentation
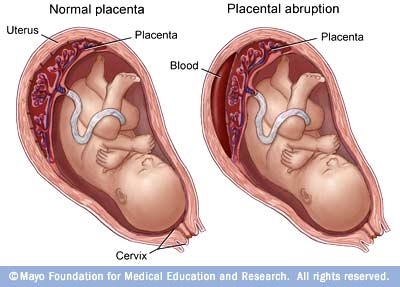
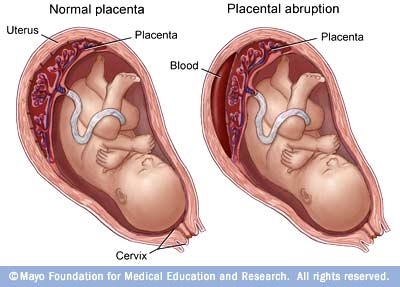
- Abruptio Placentae
- partial or total separation of the placenta from the uterine wall
- 2nd most common cause of fetal death
- vaginal bleeding occurs in 70%
- other signs include abdominal pain, uterine tenderness, frequent uterine contractions, uterine
irritability/tetany
- uterine ultrasound may be helpful in diagnosis, but it is not definitive
- late in pregnancy, abruption may occur following minor injuries
- Uterine Rupture
- suggested by abdominal tenderness, guarding, rebound tenderness, shock
- other abnormal findings include abnormal fetal lie, easy palpation of fetal parts
- x-ray findings include free intraperitoneal air, abnormal fetal position
- Risk Factors for Fetal Loss
- maternal heart rate > 110, Injury Severity Score > 9, fetal heart rate > 160 or < 120, ejection from vehicle,
motorcycle or pedestrian collisions, and evidence of placental abruption
- fetal heart tones can be auscultated with Doppler ultrasound at 10 weeks
- continuous fetal monitoring can be performed at 20 – 24 weeks
- patients with no risk factors should have continuous fetal monitoring for 6 hours
- patients with risk factors should be continuously monitored for 24 hours
Complications
- DIC
- may occur after amniotic fluid embolization or extensive placental separation
- consumptive coagulopathy
- fibrinogen levels are elevated during pregnancy, and so a normal fibrinogen level may represent early DIC
- treatment is emergent uterine evacuation and replacement of clotting factors
- Isoimmunization
- 0.01 mL of Rh-positive blood will sensitize 70% of Rh-negative patients
- all pregnant Rh-negative trauma patients should receive Rh immunoglobulin therapy unless the
injury is remote from the uterus (distal extremity injury)
- immunoglobulin therapy (RhoGAM) should be started within 72 hours of injury
References
- ATLS, 10th ed., pgs 227 – 239
- Sabiston, 20th ed., pg 2065