Diabetic Foot Infections (DBI)
- Pathophysiology
- Neuropathic Ulcers
- result from diabetic peripheral neuropathy and loss of sensation in the toes and feet
- puncture wounds, lacerations, abrasions may go unnoticed in diabetics and result in injury, infection, and tissue loss
- neuropathic arthropathy (Charcot’s foot) leads to muscle atrophy and malformation of the joints of the foot and toes, resulting in more surface ulceration and trauma
- Ischemic Ulcers
- arterial occlusive disease often coexists in patients with diabetes
- diminished or absent pulses, hair loss, and a cool foot suggest an ischemic ulceration
- ischemic ulcers commonly arise from multilevel occlusive disease
- one or both tibial arteries are usually involved, as well as the aortoiliac or femoropopliteal segments
- most diabetics ulcers result from a combination of neuropathic and ischemic components
- Microbiology
- most DBIs are polymicrobial, with 5 – 7 different organisms involved
- MRSA is a common pathogen
- additional common pathogens include enterococci, gram-negative rods, pseudomonas, and anaerobes (clostridium species and anaerobic streptococci)
- Clinical Presentation
- wide range of presentations, from chronic non-healing wounds to necrotic, infected, gangrenous wounds
- erythema, tenderness, or edema suggests a deep space infection or osteomyelitis
- elevated blood glucose levels should also prompt a search for infection
- Evaluation
- Pulse Examination
- used to determine the contribution of ischemia to the ulceration
- if pulses are palpable at the ankle, the ulcer is likely to be neuropathic; if the femoral, popliteal, and pedal pulses are absent, then a significant ischemic component is present
- Noninvasive Studies
- important complement to the physical exam
- help to determine the degree of ischemic component present in the ulcer, and whether revascularization will improve wound healing
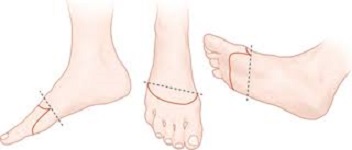
- Ankle-Brachial Index (ABI)
- ABI < 0.9 is diagnostic of arterial occlusive disease
- ABI < 0.4 is consistent with critical limb ischemia and poor wound healing
- ABI > 1.3 suggests calcified non-compressible vessels and does not reflect perfusion – additional studies will be necessary
- Toe-Brachial Index (TBI)
- more reliable indicator of perfusion in diabetics, because the small vessels are not calcified
- normal TBI is 0.7 to 0.8
- an absolute pressure > 45 mm Hg is required for wound healing in diabetics
- Transcutaneous Oxygen Measurement
- measures the absolute value of oxygen tension
- a normal value at the foot is 60 mm Hg
- values < 20 mm Hg indicate severe ischemia, and revascularization will be necessary for wound healing
- Imaging
- X-rays
- plain films are used to evaluate for bony deformity, foreign bodies, and gas in the soft tissues
- findings suggestive of osteomyelitis include cortical erosion and periosteal reaction
- MRI
- superior to plain films for diagnosing osteomyelitis
- findings characteristic of osteomyelitis include cortical destruction, bone marrow edema, and soft tissue swelling
- Lab Tests
- hemoglobin A1c levels are an indicator of diabetic control
- albumen > 3.5 predicts the ability to heal
- total lymphocyte count > 1500 is also a predictor of healing potential
- ESR and C-reactive protein are markers of inflammation and can be useful for monitoring response to therapy
- Management
- chronic ulcers, infected ulcers, and gangrene of the foot all require a separate approach
- Chronic Ulcers
- if no deep space infections are present, then minor wound debridement should be sufficient
- topical proteases (Santyl) and wet-to-dry dressings may replace or augment surgical debridement
- wound VACS are another useful healing adjunct
- Offloading
- goal is to prevent further mechanical damage to injured tissue
- specialized orthotic shoes are available for neuropathic or malformed feet
- bed rest, foot elevation, and restricted weightbearing are additional offloading strategies in more serious wounds
- Infected Ulcers
- antibiotics, debridement, amputation, and revascularization may all play a role in management
- Antibiotics
- broad-spectrum antibiotics should initially be chosen, since the infections are polymicrobial
- cultures should be obtained in the OR by tissue biopsy
- the diagnosis of osteomyelitis will require a bone biopsy
- moderate to severe infections are treated for 3 weeks
- Debridement
- source control of infection is the key step in management
- devitalized tissue is poorly vascularized, and not penetrated by antibiotics
- all deep space infections must be widely opened
- multiple procedures may be necessary
- in ambulatory patients, preserving as much viable tissue as possible is the second goal, after eradicating all infected and dead tissue
- Revascularization
- if the patient has an ulcer with a significant ischemic component, and the patient is ambulatory, then revascularization should be considered once the infection is under control
- goal is to restore pulsatile flow to the foot, usually by saphenous vein bypass to the anterior or posterior tibial arteries
- adequate inflow must also be established at the level of the common femoral and deep femoral arteries
- even after revascularization, diabetic foot ulcers are slow to heal – only 25% are healed within 6 months of surgery
- Amputation
- many patients will not be candidates for attempted limb salvage
- if the patient has no potential for ambulation, then amputation should be the primary procedure
- if the patient has significant medical comorbidities, then amputation should be the primary procedure
- extensive osteomyelitis will also often require an amputation
- Healing Adjuncts
- hyperbaric oxygen therapy facilitates healing of diabetic ulcers
- wound VACs also facilitate healing by improving local wound oxygenation, granulation, and contraction
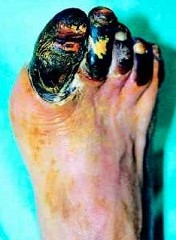
- Gangrene
- Classification
- Dry Gangrene
- not associated with infection
- emergency amputation is not indicated
- if left alone, autoamputation will occur
- Wet Gangrene
- associated with bacterial infection
- surgical emergency because sepsis and multiorgan failure may result
- Amputation
- extensive gangrene or osteomyelitis of the foot will require some level of amputation
- radical debridement will leave the patient with a nonfunctional foot
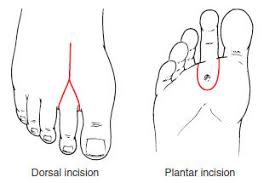
- Toe amputation
- reserved for gangrene of the middle or distal phalanges
- usually performed as a disarticulation between the proximal phalanx and metatarsal
- for a great toe amputation, preservation of the proximal phalanx aids in balance and gait
- can be done with a fish-mouth or racquet-type incision
- not indicated if the metatarsal head or forefoot is infected
- Ray Amputation
- toe amputation with partial resection of the metatarsal
- indicated when there is not enough viable tissue to cover a toe disarticulation
- usually performed with a racquet-type incision
- Transmetatarsal Amputation
- indicated for forefoot gangrene that results in significant tissue loss
- plantar flap is usually created longer than the dorsal flap
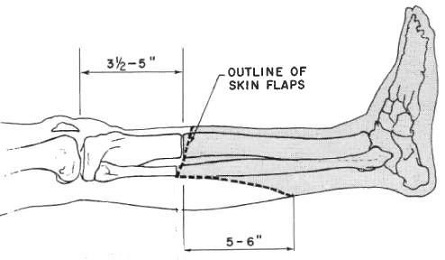
- Below Knee Amputation
- indicated when foot salvage is not possible
- usually performed with a long posterior flap
- anterior incision is made 10 cm distal to the tibial tuberosity and extended medially and laterally for two thirds of the circumference of the calf
- posterior incision is made 12 – 15 cm below the anterior incision
- the posterior muscle flap is created just deep to the tibia, and includes the soleus and gastrocnemius muscles
- neurovascular bundles should be suture ligated and divided
- a splint or knee immobilizer should be applied to prevent knee contracture
- with a prosthesis, the energy cost of ambulation increases by 30% - 60%
- in a septic patient, a guillotine amputation can be performed just above the ankle, and then revised to a formal below knee amputation after recovery
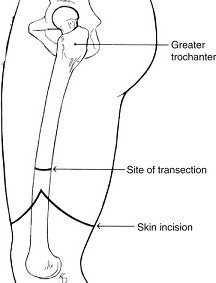
- Above Knee Amputation
- indicated for extensive infection of the lower leg
- also indicated in nonambulatory patients if healing of more distal amputations is unlikely
- in an ambulatory patient, the longer the stump, the better
- usually done with a fish-mouth incision
- energy cost of ambulation increases by 60% - 100%, which, in practical terms, means that most diabetic patients will be nonambulatory