Deep Venous Thrombosis
- Lower Extremity Venous Anatomy and Physiology
- Anatomy
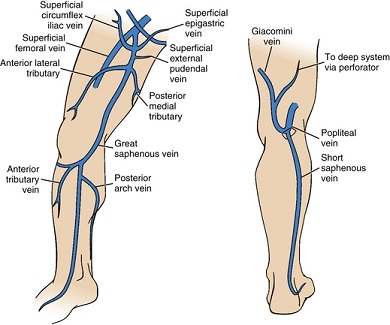
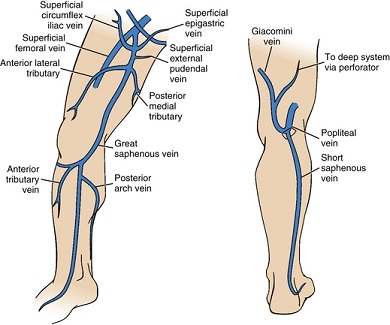
- Superficial Veins
- composed of the greater and lesser saphenous veins
- large, relatively thick-walled structures lying above the deep fascia
- lesser saphenous vein ascends posterior to the lateral malleolus and terminates in
the popliteal vein
- greater saphenous vein ascends medially and empties into the common femoral vein
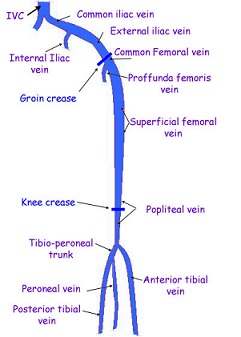
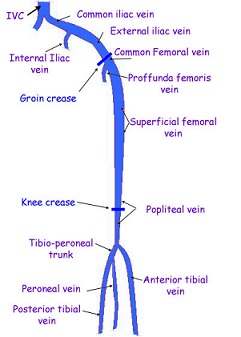
- Deep Veins
- primarily responsible for venous return
- follow the course of the major arteries
- in the lower leg the veins are paired and join at the knee to form the popliteal vein
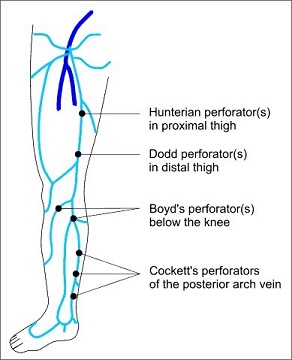
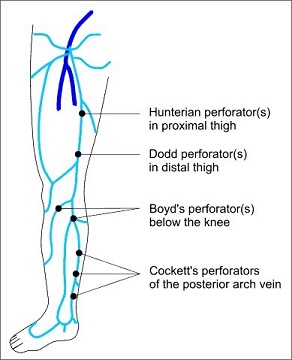
- Perforating Veins
- connect the superficial and deep systems
- contain valves that direct flow from the superficial to the deep veins
- Valves
- bicuspid valves are located within a dilated sinus of the lower extremity veins
- valves direct blood flow centrally and prevent reflux of venous blood, especially
during standing and ambulation
- more valves are located distally than proximally
- common iliac vein and vena cava do not have valves
- Physiology
- Venous Return
- Supine Position
- lower extremity venous return depends primarily on the respiratory cycle
- during inspiration, intraabdominal pressure increases and decreases
venous return
- valve closure prevents reflux of blood
- during expiration, venous return is increased as a result of the decreased
intraabdominal pressure
- Upright Position
- as a result of hydrostatic forces, the standing venous pressure in the foot
veins is 80 to 90 mm Hg
- calf muscle pump is necessary to overcome these hydrostatic forces
- when the soleus and gastrocnemius muscles contract, blood in the deep veins
is propelled centrally
- valves in the perforating veins prevent flow of blood from the deep to
the superficial veins
- Etiology
- Virchow’s triad: venous stasis, endothelial damage, and hypercoagulability
- Stasis
- most important factor for surgical patients
- general anesthesia causes a significant reduction in flow in the lower extremities
- prolonged bedrest also increases the incidence of DVT
- stasis alone is not sufficient to cause DVT: aging, obesity, malignancy, trauma, shock,
congestive heart failure, and infection are contributory factors
- Endothelial Damage
- can occur in collapsed vessels when the intimal walls are in contact
- also may occur from central venous catheters or hip arthroplasty
- in most cases of DVT, the role of endothelial injury is questionable because the DVT often
occurs in veins remote from the site of operation
- Hypercoagulability
- in experimental systems, stasis and endothelial injury alone are not sufficient to cause
thrombosis in the absence of activated clotting factors
- hereditary hypercoagulable conditions include antithrombin III deficiency, Protein C and
S deficiency
- acquired hypercoagulable conditions include malnutrition, nephrotic syndrome, malignancy,
pregnancy, use of oral contraceptives
- surgery reduces antithrombin III, suppresses plasma fibrinolytic activity, and releases
large amounts of prothrombotic tissue factor into the circulation
- Pathophysiology
- in most cases, spontaneous clot lysis occurs, and the vessel lumen is recanalized
- damage to the venous valves results in chronic venous insufficiency in 50% of patients with DVT
- most feared complication of DVT is pulmonary embolism, which accounts for over 100,000 deaths per
year in the U.S.
- Clinical Manifestations
- only 40% of patients have clinical signs of DVT
- first manifestation of a DVT may be a pulmonary embolus
- calf tenderness may be elicited by Homan’s test (dorsiflexing the foot) but the false-positive rate
is high (30%)
- swelling is often not present in calf vein thrombosis because the veins are paired, and the
obstruction is usually not complete
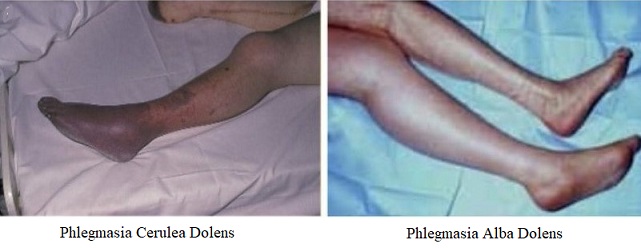
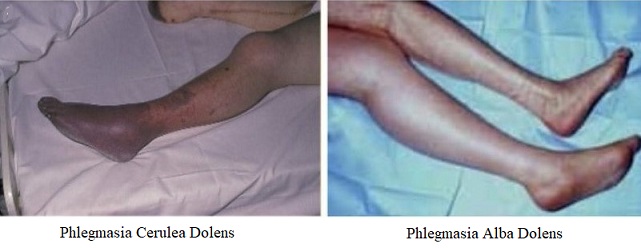
- iliofemoral thrombosis may present with massive swelling of the entire leg – phlegmasia alba dolens
- phlegmasia cerulea dolens occurs when venous thrombosis impedes most of the venous return from the
leg, ultimately causing cessation of arterial flow
- Diagnosis
- Venous Duplex Ultrasonography
- 90% accurate in diagnosing DVT
- may be performed at the bedside
- 3 elements to the venous duplex scan: 1) thrombus visualization, 2) vein compressibility,
3) venous flow analysis
- thrombus may be difficult to visualize in its acute form
- veins filled with thrombus do not compress

- Venography
- most accurate test, but it is invasive and requires the use of contrast
- main indication is when clinical suspicion is high, and the duplex scan is not definitive
- MRI
- useful for imaging the iliac veins and IVC, which are not well-visualized by duplex ultrasound
- Prophylaxis
- Risk Factors for DVT
- Medical
- previous DVT or PE
- age > 40
- pregnancy
- malignancy
- hormonal therapy
- obesity
- hypercoagulable state
- Surgical
- general anesthesia
- laparoscopic procedures
- major abdominal or pelvic surgery
- hip or knee replacement
- closed head injury, spinal cord injury, paralysis
- pelvic fractures, extremity fractures
- prolonged immobilization
- Mechanical Prophylaxis
- Ambulation
- activates the calf pump mechanism
- when sitting, the legs should be elevated to avoid venous pooling
- Sequential Compression Devices (SCDs)
- sleeves intermittently inflate with a gradient pressure from the ankle to the thigh
- replicates the calf pump mechanism
- some studies suggest that they also increase fibrinolytic activity
- compliance is an issue because many patients complain that they are uncomfortable
- often combined with graded compression stockings
- high risk patients will also receive pharmacologic prophylaxis
- Pharmacologic Prophylaxis
- Low-Dose Heparin
- 5000 U preop and then bid or tid
- prevents ~ 50% of all PE’s and 66% of all DVTs
- enhances antithrombin III activity, which inhibits factor Xa
- does not increase the rate of major hemorrhage, but wound hematomas occur in ~ 2%
of patients
- another complication is heparin-induced thrombocytopenia (HIT)
- has largely been replaced by Lovenox
- Enoxaparin (Lovenox)
- low molecular weight heparin polymer (LMWH)
- has increased bioavailability, longer half-life, increased antithrombotic activity
when compared to standard heparin
- incidence of thrombocytopenia is lower than in those receiving standard heparin
- in trauma patients, it is superior to low-dose heparin in preventing DVT
- also superior to mechanical prophylaxis in preventing DVT
- Fondaparinux (Arixtra)
- factor Xa inhibitor
- often used in patients with a history of HIT
- Treatment
- Medical Treatment
- goals are to minimize the risk of PE, limit further thrombosis, and facilitate resolution
of existing thrombi to avoid chronic venous insufficiency
- Anticoagulation
- historical treatment has been IV heparin (4 – 5 days) followed by long-term
Coumadin (3 months)
- heparin is initially given as a bolus injection and the therapeutic level is
maintained by a continuous infusion
- adequate anticoagulation is necessary in the first 24 – 48 hours of treatment in
order to prevent a high incidence of recurrent disease
- to minimize bleeding complications, the dose of heparin should be adjusted to keep
the PTT between 1.5 – 2.0 times control
- the dose of Coumadin should be adjusted to keep the INR between 2.5 – 3.0
- use of low-molecular-weight heparins appears to be as effective as standard heparin
and can be done on an outpatient basis with no need for laboratory monitoring
- other effective treatment options include subcutaneous Lovenox, subcutaneous fondaparinux,
or oral factor Xa inhibitors for a period of 3 – 6 months
- Thrombolysis
- reserved for patients with phlegmasia cerulea dolens
- goal is to completely eliminate the thrombus and maintain valvular function
- systemic thrombolysis has a high rate of incomplete thrombolysis and bleeding
complications
- catheter-directed thrombolysis is associated with better results and less bleeding
complications
- catheter-directed thrombolysis also has had good results in subclavian vein thrombosis
- Surgical Therapy
- Thrombectomy
- reserved for limb salvage in the presence of phlegmasia cerulea dolens
- the use of a small arteriovenous fistula after iliofemoral thrombectomy may reduce
the incidence of early rethrombosis
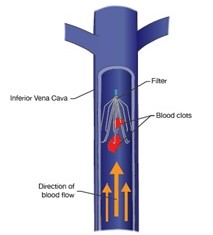
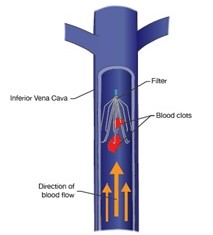
- Vena Caval Filters
- indicated when there is a failure of or contraindication to anticoagulation (recent surgery,
hemorrhagic stroke, GI bleeding)
- goal is to provide filtration of clot without occlusion of the infrarenal IVC
- percutaneous transvenous approach (Greenfield filter) is the technique of choice
- retrievable filters now exist for patients who only require short-term caval protection
Pulmonary Thromboembolism (PE)
- Pathophysiology
- PEs are usually multiple, with the lower lobes involved in most cases
- Infarction
- results from small thrombi lodging distally in the segmental and subsegmental vessels
- Abnormal Gas Exchange
- obstruction of pulmonary arteries alters the ventilation/perfusion ratio (increases dead space ventilation)
- Obstructive Shock
- pulmonary artery obstruction leads to increased pulmonary vascular resistance, which in turn results in
right ventricle outflow obstruction
- ultimately, decreased right ventricular output leads to reduced left ventricular preload and
reduced cardiac output
- Clinical Presentation
- most common presenting symptom is dyspnea
- pleuritic chest pain and cough are also common symptoms
- some patients may present with cardiogenic shock
- a surprisingly large number of patients may be asymptomatic
- Diagnosis
- CT Angiography
- PE is diagnosed by the presence of filling defects in pulmonary vessels
- CTA has excellent sensitivity and specificity (99%) for the large central pulmonary vessels

- Echocardiogram
- transthoracic or transesophageal
- primarily used when the patient is too unstable for a CTA
- findings of right heart failure or pulmonary hypertension are highly suggestive of PE
- sometimes the clot can be visualized directly
- D-Dimer
- degradation product of the fibrinolytic system
- negative D-dimer test effectively rules out a PE or DVT
- since D-dimer may be elevated in post-op patients, a positive D-dimer does not rule in a
PE/DVT in this population
- Treatment
- Anticoagulation
- prevents additional thrombus formation
- if there are no contraindications to anticoagulation, heparin or LMWH may be started
empirically before a diagnosis is established
- patients will require long-term coumadin or subcutaneous LMWH
- patients with contraindications to anticoagulation will require an IVC filter
- Thrombolytic Therapy
- may be indicated in cases of massive PE, in which more rapid clot lysis may be lifesaving
- recent surgery is a relative contraindication
- may be given systemically or via a percutaneously-placed catheter
- Pulmonary Embolectomy
- may be indicated in cases of massive PE, in which more rapid clot lysis may be lifesaving
- may be performed surgically or transcatheter, depending upon local expertise
- surgery requires a median sternotomy and cardiopulmonary bypass
- Complications
- untreated PE has a mortality rate of up to 30%, which is significantly reduced by anticoagulation
- chronic pulmonary hypertension occurs as a late outcome in a small percentage of patients
References
- Sabiston, 20th ed., pgs 1827 – 1833, 1840 – 1846
- Schwartz, 10th ed., pgs 915 – 929
- Cameron, 13th ed., pgs 1072 – 1088
- UpToDate. Overview of the Treatment of Lower Extremity Deep Vein Thrombosis. Gregory YH Lip, MD, FRCPE, FESC, FACC,
Russell D. Hull, MBBS, MSc. May 07, 2020. Pgs 1 – 27
- UpToDate. Overview of Acute Pulmonary Embolism in Adults. B. Taylor Thompson, MD, Christopher Kabrhel, MD, MPH.
Jun 09, 2020. Pgs 1 – 23