Acute Mesenteric Ischemia
- Anatomy
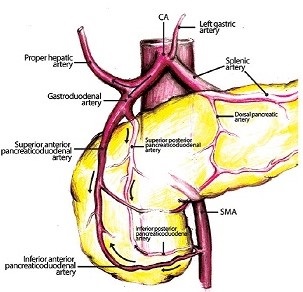
- Arterial Circulation
- 3 main arteries supply the GI tract
- there is an extensive collateral network between these arteries
- Celiac Artery (CA)
- supplies the foregut – distal esophagus, stomach, liver, spleen, duodenum
- arises from the ventral aspect of the infradiaphragmatic aorta
- surgical exposure requires division of the crura and median arcuate ligament
- Superior Mesenteric Artery (SMA)
- supplies the midgut – from the jejunum to the mid transverse colon
- arises from the ventral infradiaphragmatic aorta just below the celiac artery
- on angiography, to fully visualize the origins of the CA and SMA, a lateral view must be obtained,
as well as an AP view
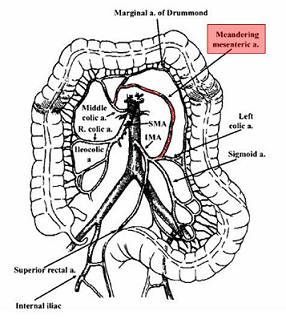
- Inferior Mesenteric Artery
- supplies the hindgut – from the mid transverse colon to the rectum
- arises from the lateral aspect of the of the infrarenal aorta
- Collateral Circulation
- superior and inferior pancreaticoduodenal arteries are the primary collateral network between the CA and SMA
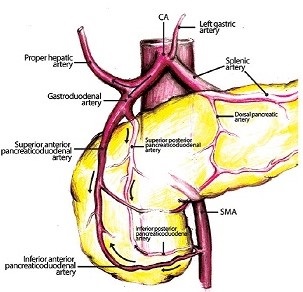
- the SMA and IMA are linked by the arc of Riolan centrally, the marginal artery of Drummond on the periphery
of the colon, and unnamed retroperitoneal vessels
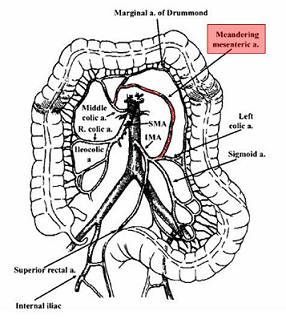
- the IMA and systemic circulation are linked by the internal iliac artery and the hemorrhoidal arteries
- Pathophysiology
- in chronic mesenteric ischemia, gradual occlusion of 2 vessels is usually tolerated because the collateral network
has time to grow and develop
- in acute mesenteric ischemia, occlusion of one main vessel is often sufficient to cause profound ischemia because
the collateral network is undeveloped
- SMA Embolus
- most common etiology of acute mesenteric ischemia (50%)
- most emboli originate from the heart as a result of atrial fibrillation or a myocardial infarction
- emboli preferentially lodge in the SMA because of its high flow rate, large diameter, and nearly parallel
course to the aorta
- most emboli lodge 3 to 10 cm distal to the SMA origin
- proximal jejunum is usually spared
- SMA Thrombosis
- accounts for 20% of cases
- occurs at the origin of the vessel
- chronic aortic and mesenteric atherosclerosis is present and patients often have a history of chronic
mesenteric ischemia (acute-on-chronic ischemia)
- involvement of at least two of the major mesenteric arteries is required for symptom development
- patients often have significant collateral circulation
- entire midgut will be ischemic
- Nonocclusive Mesenteric Ischemia
- 20% of cases
- caused by a low-flow state resulting from shock, vasopressor use, or hypovolemia
- mesenteric vessels may be normal
- mortality rate is high because of delay in diagnosis and the underlying medical condition of the patient
- Mesenteric Venous Thrombosis
- 10% of cases
- SMV is most commonly involved (70%); the portal vein, splenic vein, and IMV account for the other 30%
- venous thrombosis leads to bowel wall edema and decreased perfusion
- primary risk factors include hypercoagulable states such as protein C or protein S deficiency
- secondary risk factors include malignancy or recent abdominal surgery (splenectomy)
- Clinical Presentation
- SMA Embolus
- sudden, severe periumbilical pain out of proportion to the physical exam
- nausea/vomiting and bowel emptying are common, but bloody diarrhea is rare
- many patients are in atrial fibrillation or have had a recent MI
- SMA Thrombosis
- symptoms are often less dramatic than for an SMA embolus
- patients typically have a history of intestinal angina and weight loss from ‘food fear’
- patients may report worsening postprandial pain
- Nonocclusive Mesenteric Ischemia
- ischemic symptoms may be overshadowed by the patient’s underlying medical condition
- ICU patients may present with progressive abdominal distention and acidosis
- Mesenteric Venous Thrombosis
- slow to diagnose because the abdominal pain is often episodic and not very severe
- Diagnosis
- requires a high index of suspicion
- EGD and colonoscopy are of no value in the acute setting
- barium enema is contraindicated if intestinal ischemia is suspected
- Laboratory Tests
- common, but nonspecific, findings include leukocytosis, hemoconcentration, and an elevated serum lactate level
- normal lab findings do not exclude intestinal ischemia
- Plain Abdominal X-rays
- useful for ruling out a perforated viscus or intestinal obstruction
- suspicious findings for infarcted bowel include bowel wall thickening, pneumatosis intestinalis, or
portal venous gas
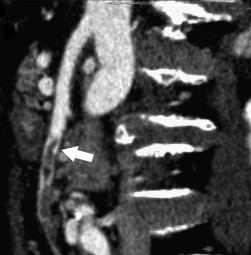
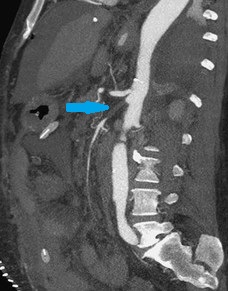
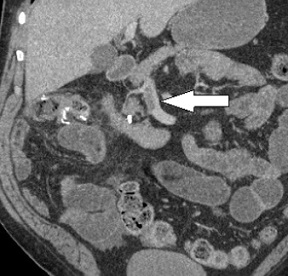
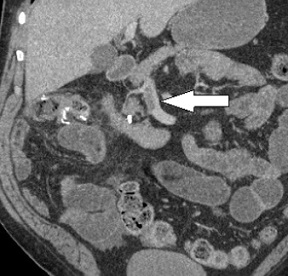
- CT Angiography
- definitive diagnostic study and should be ordered promptly if mesenteric ischemia is suspected
- should be done without oral contrast, which can obscure the mesenteric vessels and obscure bowel wall enhancement
- emboli show an abrupt cutoff several centimeters from the SMA origin, typically at the middle colic orifice
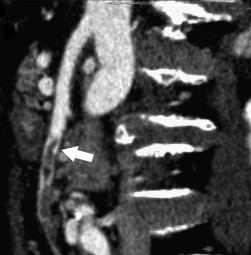
- SMA thrombosis occurs at the origin of the vessel, and extensive collateral networks are often seen
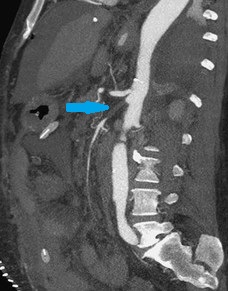
- nonocclusive mesenteric ischemia will show a normal SMA with diffuse vasospasm of the mesenteric arcades
- catheter angiography also has a therapeutic role in infusion of catheter-directed vasodilator agents

- mesenteric venous thrombosis is diagnosed by the presence of venous filling defects on delayed imaging
- Management
- Initial Management
- fluid resuscitation
- correction of metabolic acidosis, with sodium bicarbonate if necessary
- antibiotics
- systemic heparinization to prevent thrombus propagation
- avoid vasopressors if possible
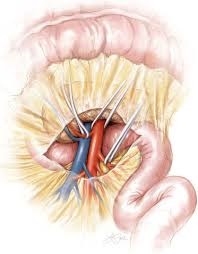
- SMA Embolus
- embolectomy proceeds bowel resection
- SMA is found at the root of the mesentery where it passes over the third portion of the duodenum
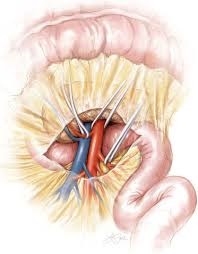
- if the artery is not diseased, a transverse arteriotomy is made; otherwise a longitudinal arteriotomy is made
- a Fogarty catheter is passed proximally and distally to remove the embolus
- a transverse arteriotomy can be closed primarily; a longitudinal arteriotomy is closed with a vein or synthetic patch
- bowel viability is assessed once flow has been restored, and obviously necrotic bowel is resected
- Doppler assessment of antimesenteric pulsations or IV fluorescein followed by Wood lamp inspection can
assist in determining bowel viability
- if bowel viability is questionable, it is left in discontinuity and a second-look procedure is done 24 – 48 hours later
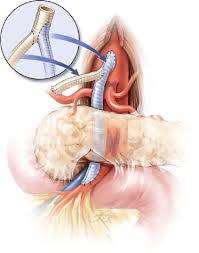
- SMA Thrombosis
- origins of the CA and SMA are severely atherosclerotic
- mesenteric bypass to a distal uninvolved segment is necessary for revascularization
- single-vessel or two-vessel bypass may be performed
- reversed saphenous vein or PTFE reinforced with rings may both be used as conduits
- may be done in an antegrade or retrograde fashion
- Antegrade Bypass
- uses the supraceliac aorta, which is usually uninvolved by atherosclerosis
- allows the use of a short graft, which resists kinking when the bowel is returned to its
normal position
- revascularization of the CA is usually performed to the common hepatic artery
- disadvantages include difficult exposure and the need for supraceliac aortic occlusion
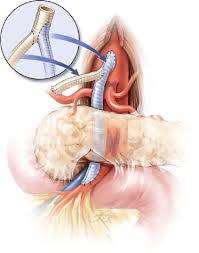
- Retrograde Bypass
- uses the infrarenal aorta or iliac artery for inflow
- advantages are the ease of exposure and no supraceliac aortic occlusion
- disadvantages include the use of inflow vessels that are usually heavily involved in atherosclerosis,
and a long graft that is easily kinked

- Nonocclusive Mesenteric Ischemia
- management is by catheter-directed infusion of a vasodilatory agent, usually papaverine
- patients are also heparinized
- all vasoconstricting agents must be stopped
- laparotomy will be required if peritonitis develops
- SMV Thrombosis
- fluid resuscitation and anticoagulation are the primary treatment modalities
- venous thrombectomy has not been shown to be effective
- surgery is limited to bowel resection in patients with peritonitis
- patients with abdominal pain but who do not have peritonitis, may benefit from catheter-directed
thrombolytic therapy
- the mesenteric venous circulation is reached by catheters placed in the splenic artery and SMA
- Endovascular Treatment
- can only be used in cases where there is a very low suspicion for gangrenous bowel
- most useful in SMA thrombosis
- catheter-directed thrombolytic therapy is first used to dissolve the thrombus
- the diseased artery may then be treated with balloon angioplasty and stenting
Chronic Mesenteric Ischemia (CMI)
- Pathophysiology
- most common cause is atherosclerotic arterial occlusive disease
- usually related to compromise of flow in both the CA and SMA
- most mesenteric atherosclerotic lesions are located at the vessel orifices
- the involvement of the mesenteric vessel is usually limited to the first 1 to 2 cm of the main trunk

- Clinical Presentation and Diagnosis
- postprandial abdominal pain (intestinal angina), ‘food fear’, and profound weight loss
- precursor to SMA thrombosis and intestinal infarction
- definitive diagnosis requires CT angiography, which will typically show occlusion of the CA and SMA at their origins
- Management
- Endovascular Procedures
- most vascular surgeons consider endovascular techniques to be procedure of choice for patients with CMI
- associated with lower rates of morbidity and mortality and shorter lengths of stay than open surgery
- long term patency rates are lower than that achieved by open surgery and more secondary procedures for
restenosis are required
- Mesenteric Bypass
- similar decision-making and technical considerations as for acute SMA thrombosis – antegrade versus
retrograde bypass
- both the CA and SMA are usually reconstructed in the chronic setting
- Transaortic Endarterectomy
- aorta is exposed with medial rotation of the viscera from the left
- U-shaped trapdoor aortotomy is made to encompass the origins of the CA and SMA
- endarterectomy is performed starting on the aorta and extending into the visceral artery orifices
- technique is most applicable to lesions limited to the first 1 to 2 cm of the visceral artery
- aortic clamp time greater than 40 to 45 minutes can result in hepatic ischemia and irreversible coagulopathy
- has largely been replace by endovascular techniques and open bypass
References
- Schwartz, 10th ed., pgs 859 – 866
- Cameron, 13th ed., pgs 1057 – 1061, 1062 - 1067
- UpToDate. Overview of Intestinal Ischemia in Adults. David A. Tender, MD, J. Thomas Lamont, MD. Jun 01, 2020.
Pgs 1 – 33
- UpToDate. Acute Mesenteric Arterial Occlusion. Gregory Pearl, MD, Ramyar Gilani, MD. Apr 07, 2020. Pgs 1 – 31