Central Venous Access
- Indications
- inadequate peripheral access
- infusion of medications that cannot be given peripherally – TPN, chemotherapy, vasopressors
- hemodynamic monitoring
- hemodialysis
- plasmapheresis
- Contraindications
- coagulopathy and thrombocytopenia are relative contraindications, depending upon the urgency of venous access
- Sites
- each possible access site has inherent advantages and disadvantages
- Internal jugular Vein
- Advantages
- low pneumothorax risk
- low risk of bleeding complications
- right side has direct access to the right atrium, making it the ideal site for
dialysis catheter placement
- Disadvantages
- risk of carotid puncture
- uncomfortable for the patient
- difficult to maintain dressings
- Femoral Vein
- Advantages
- no risk of pneumothorax
- high success rate, especially for beginners
- does not interfere with intubation or CPR
- does not require Trendelenburg positioning
- Disadvantages
- highest infection rate
- risk of ileofemoral thrombosis
- difficult for patients to ambulate
- Subclavian Vein
- Advantages
- more comfortable
- lowest infection rate
- Disadvantages
- highest risk of pneumothorax
- inability to directly tamponade bleeding
- vein is difficult to view on ultrasound
- most difficult approach for beginners
- External Jugular Vein
- Advantages
- superficial vessel that is often visible and large
- lowest risk
- Disadvantages
- can be difficult to thread a long catheter
- catheter malposition
- Catheter Placement
- Procedure location
- nontunneled catheters are usually placed at bedside
- tunneled catheters and subcutaneous ports are placed in the OR or IR suite
- Patient Monitoring
- continuous cardiac rhythm and pulse oximetry monitoring should be available
- Positioning
- the Trendelenburg position facilitates venous filling for internal jugular and subclavian vein access
and may reduce the risk of venous embolism
- however, Trendelenburg may not be tolerated by obese or critically ill patients
- Sterile Technique
- prep and drape all possible access sites
- chlorhexidine prep is superior to Betadine
- cap, mask, gown, sterile gloves for the surgeon
- systemic antibiotics are not necessary
- Use of Ultrasound (US)
- should be used whenever available and practical
- reduces the number of unsuccessful access attempts
- multiple needle passes are associated with higher rates of pneumothorax, hematoma, arterial puncture,
and nerve injury
- if ultrasound is not available, then landmarks techniques must be used
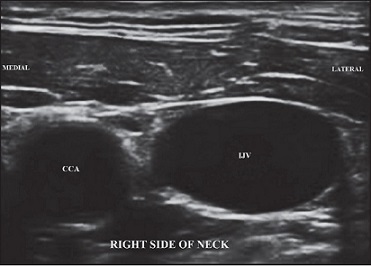
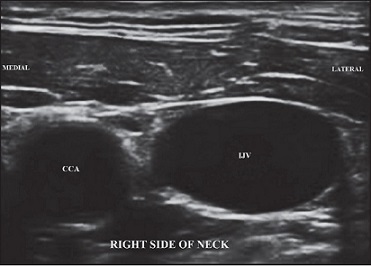
- Vein Assessment
- precannulation US can evaluate vein patency and aid in choosing the most appropriate site
- the lumen of a normal vessel is black (anechoic)
- veins are oval-shaped, thin-walled, and easily compressible
- veins also lack arterial pulsations and may have visible valves
- Dynamic Real-Time Guidance
- consists of imaging during needle placement
- static ultrasound – using the ultrasound to identify the location of the vein and then marking the
insertion site on the skin, followed by a blind stick – should not be done
- Detection of Complications
- US may allow early detection of pneumothorax and hemothorax
- Landmark Technique
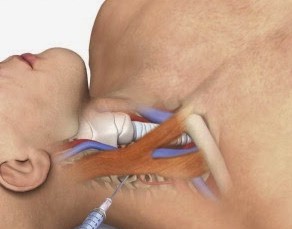
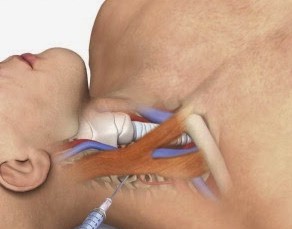
- Internal Jugular Vein
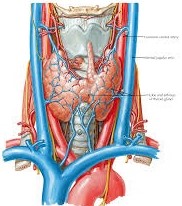
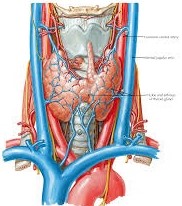
- Anatomy
- at the level of the cricoid cartilage, the IJ lies below the sternocleidomastoid muscle and is
anterolateral to the carotid artery
- at the base of the neck, the IJ is located between the two heads of the SCM
- the right IJ is preferred over the left because of its larger diameter, more direct path to the SVC
and right atrium, the lower dome of the right pleura, absence of the thoracic duct,
and easier access for a right-handed surgeon
- Approaches
- the primary surface landmarks are the anterior and posterior borders of the SCM as well as the
two heads of the SCM
- the course of the carotid artery can also be easily palpated
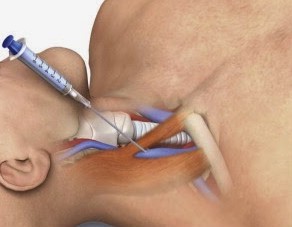
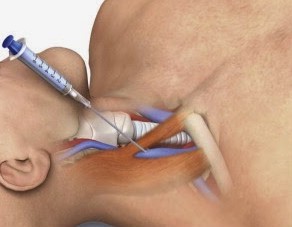
- Central Approach
- most common technique
- insertion site is at the apex of the triangle formed by the heads of the SCM
- needle is introduced lateral to the carotid pulse and directed towards the ipsilateral nipple
- Posterior Approach
- turn the head to the contralateral side
- insert the needle along the posterior border of the SCM at the junction of the middle and lower third of the muscle
- advance the needle towards the sternal notch
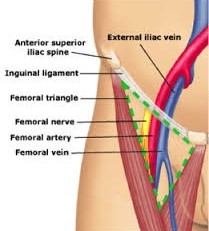
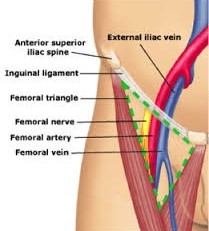
- Common Femoral Vein
- Anatomy
- the femoral vein lies within the femoral triangle, which is bordered superiorly by the inguinal
ligament, medially by the adductor longus muscle, and laterally by the sartorius muscle
- the femoral vein is medial to the femoral artery in the femoral triangle
- the insertion site will be 2 - 3 cm below the inguinal ligament and one cm medial to the femoral
artery pulse
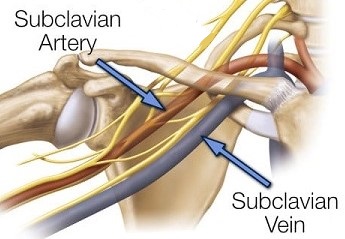
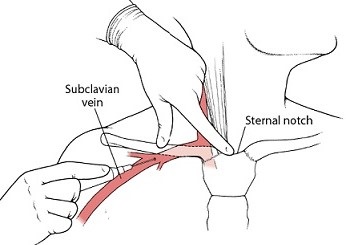
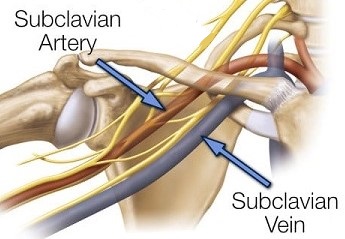
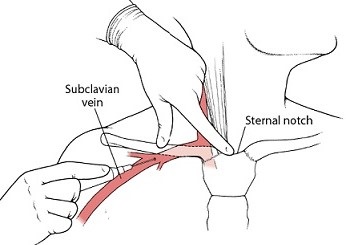
- Subclavian Vein
- Anatomy
- travels below the clavicle and above the first rib
- the bend of the clavicle is an important surface landmark
- Technique
- the insertion site is 1 – 2 cm lateral to the bend of the clavicle
- the needle is advanced until it hits the clavicle
- the thumb is then used to push the needle below the clavicle
- the needle is then slowly advanced in the direction of the sternal notch
Dialysis Access
- Access Types and Outcomes
- Types of Access
- tunneled central venous catheters
- autogenous arteriovenous fistulas
- prosthetic graft arteriovenous fistulas
- Outcomes of Access Types
- Central Tunneled Catheters
- associated with the worst outcomes and should be avoided if at all possible
- often placed while waiting for a fistula or prosthetic graft to mature
- also used in patients who develop acute renal failure that requires emergency dialysis
- Autogenous Arteriovenous Fistulas (AFs)
- associated with the best outcomes
- highest patency rates; lowest rates of thrombosis, stenosis, and infection
- however, not every patient will have a suitable vein for fistula creation
- national goal is an AF rate of 65% in new dialysis patients
- Prosthetic graft Fistulas (PFs)
- should be the second choice if an AF is not possible
- have shorter maturation times than AFs
- often technically easier to perform than AFs
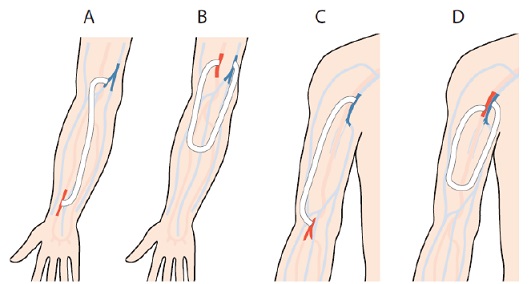
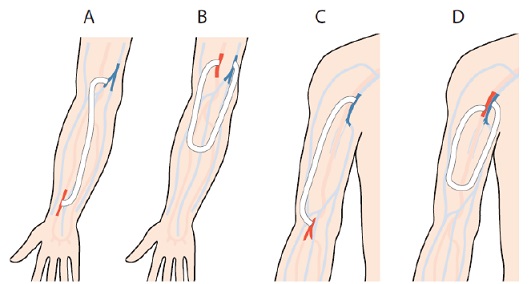
- Selecting an Access Type
- begin distally in the nondominant arm and work proximally as necessary
- AFs are preferred over PFs if the venous anatomy will support an AF
- AFs: radiocephalic, brachiocephalic, upper arm basilic transposition
- PFs: distal radial artery to brachial vein straight graft, distal brachial artery to distal
brachial vein forearm loop graft, distal brachial artery to proximal brachial vein straight graft
- may use the dominant arm if necessary
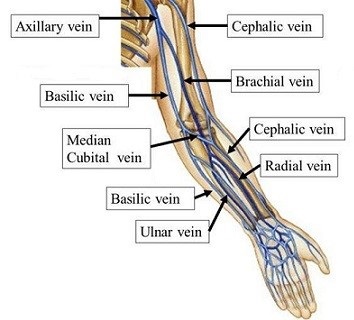
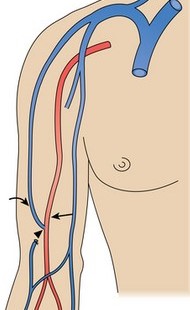
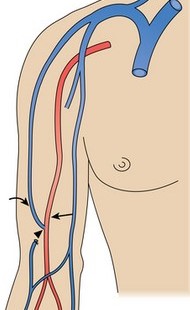
- Vascular Anatomy of the Upper Extremity
- Venous Anatomy
- Cephalic Vein
- arises from the radial aspect of the veins draining the dorsum of the hand
- in the forearm, it travels with the radius
- as it crosses the elbow, it is found in the groove between the brachioradialis and
biceps muscles
- in the upper arm, it passes between the deltoid and pectoralis major muscles
(deltopectoral groove)
- Basilic Vein
- originates from the ulnar aspect of the dorsum of the hand
- travels subcutaneously on the ulnar side of the forearm
- joined by the median antecubital vein in the antecubital fossa
- travels in the groove between the biceps muscle and the pronator teres muscles
- descends through the deep fascia, crosses the brachial artery, and then travels parallel
to the brachial artery and vein
- axillary vein is formed by the junction of the brachial and basilic veins
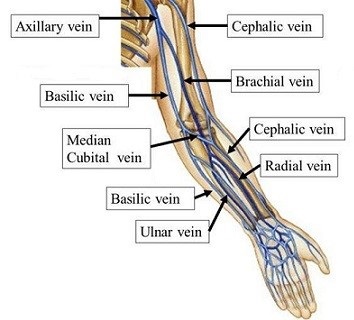
- Arterial Anatomy
- Radial and Ulnar Arteries

- Brachial Artery
- Evaluation for a New Access
- History
- need to know about previous venous access procedures, including subclavian lines, ports,
PICC lines, pacemakers, defibrillators
- prior trauma to the upper arm or clavicle should be noted
- all these procedures or prior trauma can result in central venous thrombosis or stenosis, which can make the
arm unusable for dialysis access
- PICC lines render the basilic vein unusable
- Physical Exam
- Arteries
- brachial, radial, ulnar pulses should be palpated bilaterally
- Allen’s test to confirm adequacy of ulnar flow to the hand should be done if a
radiocephalic fistula is planned
- Veins
- a tourniquet is used to assess the superficial veins of the forearm
- for a successful radiocephalic fistula, the cephalic vein should be palpable from the
wrist to the antecubital fossa
- physical exam cannot assess adequacy of central venous outflow
- Duplex Ultrasound
- Venous Assessment
- particularly valuable in obese patients or intravenous drug abusers
- superficial veins of the forearm are assessed for diameter, compressibility, and
continuity with upper arm veins
- patency of the deep system and continuity with patent axillary and subclavian veins
must be confirmed
- Arterial Assessment
- target artery should be > 2.0 mm in diameter
- palmar arch must be patent
- no proximal stenosis
- Venography
- main role is to confirm central vein patency, if the Duplex scan is nonconfirmatory
- Dialysis Catheters
- Non-cuffed Catheters
- used when emergency dialysis is necessary or if the length of dialysis is likely to be less
than 3 weeks
- may be placed at the bedside
- internal jugular vein is preferred over the subclavian vein
- femoral vein catheters may be used on a temporary emergent basis if upper extremity access is
unsuccessful or unavailable
- Cuffed Catheters
- most common indication is for immediate dialysis while awaiting an AF to mature (6 – 12 weeks)
- contralateral internal jugular vein is the preferred site because it minimizes the risk of
ipsilateral venous outflow obstruction
- Autogenous Fistulas
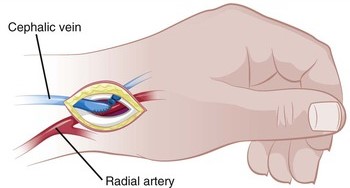
- Forearm Fistulas
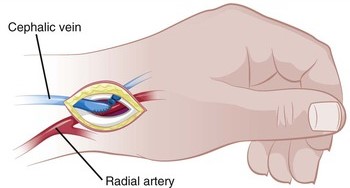
- Radiocephalic Fistula
- most commonly performed AF, but has the lowest technical success and maturation rates
- cephalic vein is dissected out and then divided
- a spatulated end-to-side anastomosis is created
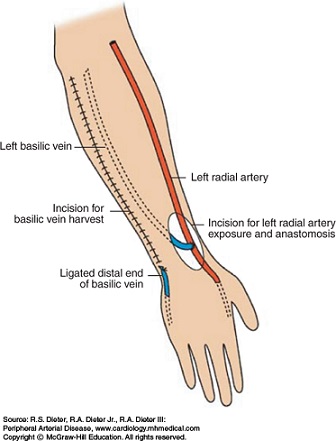
- Forearm Venous Transpositions
- many patients will not have a suitable cephalic vein in close proximity to the radial
artery
- Duplex mapping can identify suitable-sized forearm veins located in a deeper
subcutaneous location
- if left in situ, cannulating these veins with a dialysis needle may be difficult
- these veins can then be mobilized and transposed through a subcutaneous tunnel to a
more readily accessible location on the forearm
- Upper Arm Fistulas
- generally chosen after a failed forearm fistula or graft
- usually performed with cephalic or basilic vein transposition, which allows more convenient
dialysis access
- patency rates are superior to prosthetic grafts
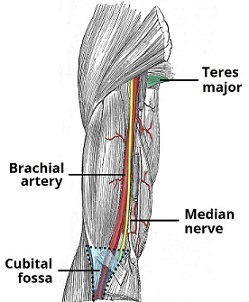
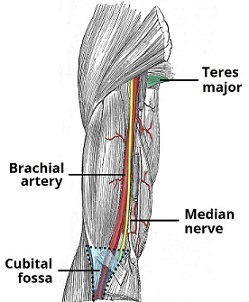
- Brachiocephalic Fistula
- cephalic vein is found in the groove between the brachioradialis and biceps muscles,
and is in close proximity to the musculocutaneous nerve
- cephalic vein is divided in the antecubital fossa and tunneled in the subcutaneous plane
over to the brachial artery
- brachial artery is exposed in the antecubital fossa
- end-to-side anastomosis is performed
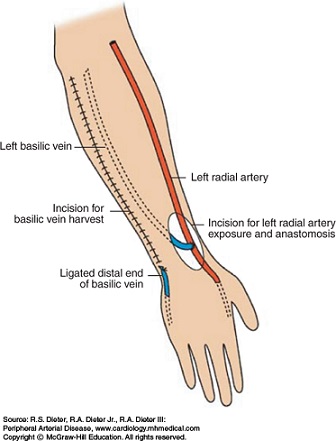
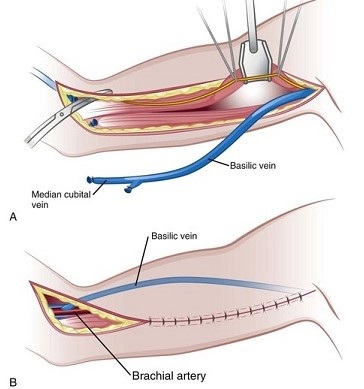
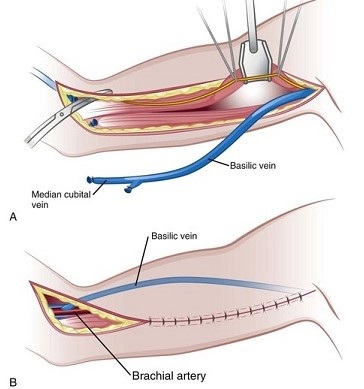
- Brachiobasilic Fistula
- chosen if the cephalic vein is not usable or of sufficient size
- vein is located anterior to the medial epicondyle of the humerus, and is mobilized to
its junction with the brachial vein
- vein is divided distally and tunneled subcutaneously to the brachial artery
- Prosthetic Fistulas
- if there is no suitable vein for autogenous access, then a prosthetic graft must be used
- a good graft is better than a bad vein
- most commonly used graft is 6 mm PTFE
- Failing or Failed Access
- Dialysis Catheters
- usually present with poor flows during dialysis or arm swelling
- Duplex ultrasound will identify central venous thrombosis, which mandates catheter removal
- if there is no central venous obstruction, transcatheter thrombolytic therapy can be effective
- malpositioned catheters can be repositioned endovascularly
- catheter tips encapsulated in fibrin sheaths can also be managed endovascularly
- if the catheter cannot be salvaged, a new one must be placed
- Autogenous Fistulas and Prosthetic Grafts
- early failure is usually related to technical problems
- most late graft failures are caused by intimal hyperplasia at the venous anastomosis
- high venous pressures, poor arterial inflow, recirculation, and diminishing effectiveness of
dialysis all indicate an access problem
- a lack of bruit or thrill indicates thrombosis
- a weak thrill or bruit suggests an inflow problem
- pulsatility in a fistula suggests an outflow problem
- fistulogram is both diagnostic and therapeutic
- thrombectomy, balloon dilation of venous outflow stenoses, and stenting may be performed at the
time of the fistulogram
- open options include patch angioplasty or anastomotic revision
- Complications of Dialysis Access
- Infection
- most frequent complication
- 30% of deaths in dialysis patients are related to infections
- risk: catheters > prosthetic grafts > fistulae
- infected catheters must be removed or exchanged
- infected grafts usually must be removed; occasionally, one can be salvaged by removal and
replacement of a portion of the graft
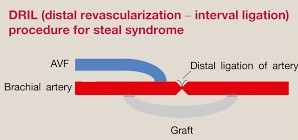
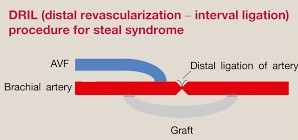
- Arterial Insufficiency (Steal Syndrome)
- fistulae and grafts create a low-resistant circuit that shunts arterial flow into the
low-pressure venous outflow
- in addition, flow in the artery distal to the access site may become retrograde
- brachial artery-based accesses have the highest risk
- typical symptom is a cold or painful hand; if untreated, tissue loss may occur
- if the patient has a radial artery-based fistula, ligation of the artery distal to the fistula
restores flow in the palmar arch through the ulnar artery
- for brachial artery-based fistulas, distal revascularization with interval ligation
revascularizes the distal limb and preserves the access
References
- UpToDate. Overview of Central Venous Access in Adults. Alan C. Heffner, MD, Mark P. Androes, MD. Mar 19, 2020.
Pgs 1 – 22
- UpToDate. Principles of Ultrasound-Guided Venous Access. Jeremiah J. Sabado, MD, Mauro Pittiruti, MD. Apr 06, 2020. Pgs 1 – 41
- Sabiston, 20th ed., pgs 1796 – 1805
- Cameron, 13th ed., pgs 1067 - 1072